Arthritis of the Foot and Ankle
Arthritis is inflammation of one or more of your joints. It can cause pain and stiffness in any joint in the body, and is common in the small joints of the foot and ankle.
There are more than 100 forms of arthritis, many of which affect the foot and ankle. All types can make it difficult to walk and perform activities you enjoy.
Although there is no cure for arthritis, there are many treatment options available to slow the progress of the disease and relieve symptoms. With proper treatment, many people with arthritis are able to manage their pain, remain active, and lead fulfilling lives.
Anatomy
 During standing, walking, and running, the foot and ankle provide support, shock absorption, balance, and several other functions that are essential for motion. Three bones make up the ankle joint, primarily enabling up and down movement. There are 28 bones in the foot, and more than 30 joints that allow for a wide range of movement.
During standing, walking, and running, the foot and ankle provide support, shock absorption, balance, and several other functions that are essential for motion. Three bones make up the ankle joint, primarily enabling up and down movement. There are 28 bones in the foot, and more than 30 joints that allow for a wide range of movement.
In many of these joints the ends of the bones are covered with articular cartilage—a slippery substance that helps the bones glide smoothly over each other during movement. Joints are surrounded by a thin lining called the synovium. The synovium produces a fluid that lubricates the cartilage and reduces friction.
Tough bands of tissue, called ligaments, connect the bones and keep the joints in place. Muscles and tendons also support the joints and provide the strength to make them move.
Description
The major types of arthritis that affect the foot and ankle are osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis
Osteoarthritis, also known as degenerative or “wear-and-tear” arthritis, is a common problem for many people after they reach middle age, but it may occur in younger people, too.
In osteoarthritis, the cartilage in the joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful osteophytes (bone spurs).
In addition to age, other risk factors for osteoarthritis include obesity and family history of the disease.
Osteoarthritis develops slowly, causing pain and stiffness that worsen over time.
Rheumatoid arthritis
 Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages the bone and cartilage, as well as ligaments and tendons, and may cause serious joint deformity and disability.
The exact cause of rheumatoid arthritis is not known. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a “trigger,” such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joints.
Posttraumatic Arthritis
Posttraumatic arthritis can develop after an injury to the foot or ankle. Dislocations and fractures—particularly those that damage the joint surface—are the most common injuries that lead to posttraumatic arthritis. Like osteoarthritis, posttraumatic arthritis causes the cartilage between the joints to wear away. It can develop many years after the initial injury.
An injured joint is about seven times more likely than an uninjured joint to become arthritic, even if the injury is properly treated. In fact, following an injury, your body may actually secrete hormones that stimulate the death of your cartilage cells.
Symptoms
The symptoms of arthritis vary depending on which joint is affected. In many cases, an arthritic joint will be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There can be other symptoms, as well, including:
- Pain with motion
- Pain that flares up with vigorous activity
- Tenderness when pressure is applied to the joint
- Joint swelling, warmth, and redness
- Increased pain and swelling in the morning, or after sitting or resting
- Difficulty in walking due to any of the above symptoms
Doctor Examination
Physical Examination
Your doctor will discuss your overall health and medical history and ask about any medications you may be taking. He or she will examine your foot and ankle for tenderness and swelling and ask questions to understand more about your symptoms. These questions may include:
- When did the pain start?
- Where exactly is the pain? Does it occur in one foot or in both feet?
- When does the pain occur? Is it continuous, or does it come and go?
- Is the pain worse in the morning or at night? Does it get worse when walking or running?
Your doctor will also ask if you have had an injury to your foot or ankle in the past. If so, he or she will discuss your injury, including when it occurred and how it was treated.
Your doctor will also examine your shoes to determine if there is any abnormal or uneven wear and to ensure that they are providing sufficient support for your foot and ankle.
Gait analysis. During the physical examination, your doctor will closely observe your gait (the way you walk). Pain and joint stiffness will change the way you walk. For example, if you are limping, the way you limp can tell your doctor a lot about the severity and location of your arthritis.
During the gait analysis, your doctor will assess how the bones in your leg and foot line up when you walk, measure your stride, and test the strength of your ankles and feet.
Tests

X-rays. These imaging tests provide detailed pictures of dense structures such as bone. An x-ray of an arthritic foot may show narrowing of the joint space between bones (an indication of cartilage loss), changes in the bone (such as fractures), or the formation of bone spurs.
Weight-bearing x-rays are taken while you stand. They are the most valuable additional test in diagnosing the severity of arthritis and noting any joint deformity associated with it. In arthritic conditions, if x-rays are taken without standing, it is difficult to assess how much arthritis is present, where it is located in the joint, and how much deformity is present. So, it is very important that, when possible, x-rays are taken standing.
Other imaging tests. In some cases, a bone scan, computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan may be needed to determine the condition of the bone and soft tissues.
Laboratory tests. Your doctor may also recommend blood tests to determine which type of arthritis you have. With some types of arthritis, including rheumatoid arthritis, blood tests are important for an accurate diagnosis.
Your doctor may refer you to a rheumatologist if he or she suspects rheumatoid arthritis. Although your symptoms and the results from a physical examination and tests may be consistent with rheumatoid arthritis, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Nonsurgical Treatment
Initial treatment of arthritis of the foot and ankle is usually nonsurgical. Your doctor may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can help relieve the pain of arthritis and slow the progression of the disease. These changes include:
- Minimizing activities that aggravate the condition.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) to lessen the stress on your foot and ankle.
- Losing weight to reduce stress on the joints, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your foot and ankle. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Although physical therapy often helps relieve stress on the arthritic joints, in some cases it may intensify joint pain. This occurs when movement creates increasing friction between the arthritic joints. If your joint pain is aggravated by physical therapy, your doctor will stop this form of treatment.

Assistive devices. Using a cane or wearing a brace—such as an ankle-foot orthosis (AFO)-may help improve mobility. In addition, wearing shoe inserts (orthotics) or custom-made shoes with stiff soles and rocker bottoms can help minimize pressure on the foot and decrease pain. In addition, if deformity is present, a shoe insert may tilt the foot of ankle back straight, creating less pain in the joint.
Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce swelling and relieve pain. In addition, cortisone is a very effective anti-inflammatory agent that can be injected into an arthritic joint. Although an injection of cortisone can provide pain relief and reduce inflammation, the effects are temporary.
Surgical Treatment
Your doctor may recommend surgery if your pain causes disability and is not relieved with nonsurgical treatment. The type of surgery will depend on the type and location of the arthritis and the impact of the disease on your joints. In some cases, your doctor may recommend more than one type of surgery.
Arthroscopic debridement. This surgery may be helpful in the early stages of arthritis. Debridement (cleansing) is a procedure to remove loose cartilage, inflamed synovial tissue, and bone spurs from around the joint.
 During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your foot or ankle joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments. Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for a traditional, open surgery.
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your foot or ankle joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments. Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for a traditional, open surgery.
Arthroscopic surgery is most effective when pain is due to contact between bone spurs and the arthritis has not yet caused significant narrowing of the joint space between the bones. Arthroscopy can make an arthritic joint deteriorate more rapidly. Removing bone spurs may increase motion in the joint, causing the cartilage to wear away quicker.
Arthrodesis (fusion). Arthrodesis fuses the bones of the joint completely, making one continuous bone out of two or more bones. The goal of the procedure is to reduce pain by eliminating motion in the arthritic joint.
 During arthrodesis, the doctor removes the damaged cartilage and then uses pins, plates and screws, or rods to fix the joint in a permanent position. Over time, the bones fuse or grow together, just like two ends of a broken bone grow together as it heals. By removing the joint, the pain disappears.
During arthrodesis, the doctor removes the damaged cartilage and then uses pins, plates and screws, or rods to fix the joint in a permanent position. Over time, the bones fuse or grow together, just like two ends of a broken bone grow together as it heals. By removing the joint, the pain disappears.
Arthrodesis is typically quite successful, although there can be complications. In some cases, the joint does not fuse together (nonunion), and the hardware may break. This may happen if you put weight on your foot before the fusion is complete. While the broken hardware does not cause pain, the nonunion of the fusion can lead to pain and swelling. If nonunion occurs, a second operation to place bone graft in the ankle and place new hardware may be needed. However, repeated fusions are not as likely to be successful, so it is best to closely follow your doctor’s guidelines during the recovery period of your original operation.
 A small percentage of patients have problems with wound healing, but these problems can usually be addressed by bracing or by an additional surgery. In some cases, loss of motion in the ankle after a fusion causes the joints adjacent to the one fused to bear more stress than they did before the surgery. This can lead to arthritis in the adjacent joints years after the surgery.
A small percentage of patients have problems with wound healing, but these problems can usually be addressed by bracing or by an additional surgery. In some cases, loss of motion in the ankle after a fusion causes the joints adjacent to the one fused to bear more stress than they did before the surgery. This can lead to arthritis in the adjacent joints years after the surgery.
Total ankle replacement (arthroplasty). In total ankle replacement, your doctor removes the damaged cartilage and bone, and then positions new metal or plastic joint surfaces to restore the function of the joint.
Although total ankle replacement is not as common as total hip or total knee replacement, advances in implant design have made it a viable option for many people.
Ankle replacement is most often recommended for patients who have:
- Advanced arthritis of the ankle
- Arthritis that has destroyed the ankle joint surfaces
- Ankle pain that interferes with daily activities
Ankle replacement relieves the pain of arthritis and offers patients more mobility and movement than fusion. In addition, being able to move the formerly arthritic joint means that less stress is transferred to the adjacent joints. This lessens the chance of developing adjacent joint arthritis.
As in any type of joint replacement, an ankle implant may loosen or fail over the years. If the implant failure is severe, the replaced joint can be exchanged for a new implant — this procedure is called a revision surgery.
Another option is to remove the implant and fuse the joint. This type of fusion is more difficult than when fusion is done as the initial procedure. When the implant is removed, there is space in the bone that must be filled with bone graft to maintain the length of the leg. Because the new bone may not be as strong, the risk of nonunion is greater.
Recovery
In most cases, surgery relieves the pain of arthritis and makes it easier to perform daily activities. Full recovery can take from 4 to 9 months, depending on the severity of your condition before surgery and the complexity of your procedure.
Foot and ankle surgery can be painful. While you should expect to feel some discomfort, advancements in pain control now make it easier for your doctor to manage and relieve pain. Immediately after surgery, you will be given medication for pain relief. If needed, your doctor will provide you with a pain reliever that you can take for a short time while you are home.
Your doctor will most likely apply a cast after surgery to limit movement in your foot and ankle and to prevent nonunion. To reduce swelling, it is important to keep your foot elevated above the level of your heart for 1 to 2 weeks after surgery.
Later in your recovery, your doctor may recommend physical therapy to help you regain strength in your foot or ankle and to restore range of motion.
In most cases, you will be able to resume your daily activities in 3 to 4 months although, for a period of time, you may need to wear supportive shoes or a brace.
Total hip replacement (also known as hip arthroplasty) is a common orthopaedic procedure and, as the population ages, it is expected to become even more common. Replacing the hip joint with an implant or “prosthesis” relieves pain and improves mobility so that you are able to resume your normal, everyday activities.
The traditional surgical approach to total hip replacement uses a single, long incision to view and access the hip joint. A variation of this approach is a minimally invasive procedure in which one or two shorter incisions are used. The goal of using shorter incisions is to reduce pain and speed recovery. Unlike traditional total hip replacement, the minimally invasive technique is not suitable for all patients. Your orthopaedic surgeon will discuss different surgical options with you.
Description
During any hip replacement surgery, the damaged bone is cut and removed, along with some soft tissues. In minimally invasive surgery, a smaller surgical incision is used and fewer muscles around the hip are cut or detached. Despite this difference, however, both traditional hip replacement surgery and minimally invasive surgery are technically demanding and have better outcomes if the surgeon and operating team have considerable experience.
Traditional Hip Replacement
To perform a traditional hip replacement:
- A 10- to 12-inch incision is made on the side of the hip. The muscles are split or detached from the hip, allowing the hip to be dislocated and fully viewed by the surgical team.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur, then a metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.

Minimally Invasive Hip Replacement
In minimally invasive total hip replacement, the surgical procedure is similar, but there is less cutting of the tissue surrounding the hip. The artificial implants used are the same as those used for traditional hip replacement. However, specially designed surgical instruments are needed to prepare the socket and femur and to place the implants properly.
Minimally invasive total hip replacement can be performed with either one or two small incisions. Smaller incisions allow for less tissue disturbance.
- Single-incision surgery. In this type of minimally invasive hip replacement, the surgeon makes a single incision that usually measures from 3 to 6 inches. The length of the incision depends on the size of the patient and the difficulty of the procedure.
The incision is usually placed over the outside of the hip. The muscles and tendons are split or detached from the hip, but to a lesser extent than in traditional hip replacement surgery. They are routinely repaired after the surgeon places the implants. This encourages healing and helps prevent dislocation of the hip.
- Two-incision surgery. In this type of minimally invasive hip replacement, the surgeon makes two small incisions:
- A 2- to 3-inch incision over the groin for placement of the socket, and
- A 1- to 2-inch incision over the buttock for placement of the femoral stem.
To perform the two-incision procedure, the surgeon may need guidance from x-rays. It may take longer to perform the two-incision surgery than it does to perform traditional hip replacement surgery.
The hospital stay after minimally invasive surgery is similar in length to the stay after traditional hip replacement surgery–ranging from 1 to 4 days. Physical rehabilitation is a critical component of recovery. Your surgeon or a physical therapist will provide you with specific exercises to help increase your range of motion and restore your strength.
Candidates for Minimally Invasive Total Hip Replacement
Minimally invasive total hip replacement is not suitable for all patients. Your doctor will conduct a comprehensive evaluation and consider several factors before determining if the procedure is an option for you.
In general, candidates for minimal incision procedures are thinner, younger, healthier, and more motivated to participate in the rehabilitation process, compared with patients who undergo the traditional surgery.
Minimally invasive techniques are less suitable for patients who are overweight or who have already undergone other hip surgeries. In addition, patients who have a significant deformity of the hip joint, those who are very muscular, and those with health problems that may slow wound healing may be at a higher risk for problems from minimally invasive total hip replacement.
Conclusion
Minimally invasive and small incision total hip replacement surgery is an evolving area and more research is needed on the long-term function and durability of the implants.
The benefits of minimally invasive hip replacement have been reported to include less damage to soft tissues, leading to a quicker, less painful recovery and more rapid return to normal activities. Current evidence suggests that the long-term benefits of minimally invasive surgery do not differ from those of hip replacement performed with the traditional approach.
Like all surgery, minimally invasive surgery has a risk of complications. These complications include nerve and artery injuries, wound healing problems, infection, fracture of the femur, and errors in positioning the prosthetic hip implants.
Like traditional hip replacement surgery, minimally invasive surgery should be performed by a well-trained, highly experienced orthopaedic surgeon. Your orthopaedic surgeon can talk to you about his or her experience with minimally invasive hip replacement surgery, and the possible risks and benefits of the techniques for your individual treatment.
There are more than 100 different forms of arthritis, a disease that can make it difficult to do everyday activities because of joint pain and stiffness.
Inflammatory arthritis occurs when the body’s immune system becomes overactive and attacks healthy tissues. It can affect several joints throughout the body at the same time, as well as many organs, such as the skin, eyes, and heart.
There are three types of inflammatory arthritis that most often cause symptoms in the hip joint:
- Rheumatoid arthritis;
- Ankylosing spondylitis; and
- Systemic lupus erythematosus.
Although there is no cure for inflammatory arthritis, there have been many advances in treatment, particularly in the development of new medications. Early diagnosis and treatment can help patients maintain mobility and function by preventing severe damage to the joint.
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and socket. It creates a smooth, low-friction surface that helps the bones glide easily across each other. The surface of the joint is covered by a thin lining called the synovium. In a healthy hip, the synovium produces a small amount of fluid that lubricates the cartilage and aids in movement.

Description
The most common form of arthritis in the hip is osteoarthritis — the “wear-and-tear” arthritis that damages cartilage over time, typically causing painful symptoms in people after they reach middle age. Unlike osteoarthritis, inflammatory arthritis affects people of all ages, often showing signs in early adulthood.
Rheumatoid Arthritis
In rheumatoid arthritis, the synovium thickens, swells, and produces chemical substances that attack and destroy the articular cartilage covering the bone. Rheumatoid arthritis often involves the same joint on both sides of the body, so both hips may be affected.
Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inflammation of the spine that most often causes lower back pain and stiffness. It may affect other joints, as well, including the hip.
Systemic Lupus Erythematosus
Systemic lupus erythematosus can cause inflammation in any part of the body, and most often affects the joints, skin, and nervous system. The disease occurs in young adult women in the majority of cases.
People with systemic lupus erythematosus have a higher incidence of osteonecrosis of the hip, a disease that causes bone cells to die, weakens bone structure, and leads to disabling arthritis.
Cause
The exact cause of inflammatory arthritis is not known, although there is evidence that genetics plays a role in the development of some forms of the disease.
Symptoms
Inflammatory arthritis may cause general symptoms throughout the body, such as fever, loss of appetite and fatigue. A hip affected by inflammatory arthritis will feel painful and stiff. There are other symptoms, as well:
- A dull, aching pain in the groin, outer thigh, knee, or buttocks
- Pain that is worse in the morning or after sitting or resting for a while, but lessens with activity
- Increased pain and stiffness with vigorous activity
- Pain in the joint severe enough to cause a limp or make walking difficult
Doctor Examination
Your doctor will ask questions about your medical history and your symptoms, then conduct a physical examination and order diagnostic tests.
Physical Examination
During the physical examination, your doctor will evaluate the range of motion in your hip. Increased pain during some movements may be a sign of inflammatory arthritis. He or she will also look for a limp or other problems with your gait (the way you walk) due to stiffness of the hip.
X-rays
X-rays are imaging tests that create detailed pictures of dense structures, like bone. X-rays of an arthritic hip will show whether there is any thinning or erosion in the bones, any loss of joint space, or any excess fluid in the joint.
Blood Tests
Blood tests may reveal whether a rheumatoid factor—or any other antibody indicative of inflammatory arthritis—is present.

Treatment
Although there is no cure for inflammatory arthritis, there are a number of treatment options that can help prevent joint destruction. Inflammatory arthritis is often treated by a team of healthcare professionals, including rheumatologists, physical and occupational therapists, social workers, rehabilitation specialists, and orthopaedic surgeons.
Nonsurgical Treatment
The treatment plan for managing your symptoms will depend upon your inflammatory disease. Most people find that some combination of treatment methods works best.
Non-steroidal anti-inflammatory drugs (NSAIDs). Drugs like naproxen and ibuprofen may relieve pain and help reduce inflammation. NSAIDs are available in both over-the-counter and prescription forms.
Corticosteroids. Medications like prednisone are potent anti-inflammatories. They can be taken by mouth, by injection, or used as creams that are applied directly to the skin.
Disease-modifying antirheumatic drugs (DMARDs). These drugs act on the immune system to help slow the progression of disease. Methotrexate and sulfasalazine are commonly prescribed DMARDs.
Physical therapy. Specific exercises may help increase the range of motion in your hip and strengthen the muscles that support the joint.
In addition, regular, moderate exercise may decrease stiffness and improve endurance. Swimming is a preferred exercise for people with ankylosing spondylitis because spinal motion may be limited.
Assistive devices. Using a cane, walker, long-handled shoehorn, or reacher may make it easier for you to perform the tasks of daily living.
Surgical Treatment
If nonsurgical treatments do not sufficiently relieve your pain, your doctor may recommend surgery. The type of surgery performed depends on several factors, including:
- Your age
- Condition of the hip joint
- Which disease is causing your inflammatory arthritis
- Progression of the disease
The most common surgical procedures performed for inflammatory arthritis of the hip include total hip replacement and synovectomy.
Total hip replacement. Your doctor will remove the damaged cartilage and bone, and then position new metal or plastic joint surfaces to restore the function of your hip. Total hip replacement is often recommended for patients with rheumatoid arthritis or ankylosing spondylitis to relieve pain and improve range of motion.

Synovectomy. Synovectomy is done to remove part or all of the joint lining (synovium). It may be effective if the disease is limited to the joint lining and has not affected the articular cartilage that covers the bones. Generally, the procedure is used to treat only the early stages of inflammatory arthritis.
Your doctor will discuss the various surgical options with you. Do not hesitate to ask why a specific procedure is being recommended and what outcome you can expect.
Complications. Although complications are possible in any surgery, your doctor will take steps to minimize the risks. The most common complications of surgery include:
- Infection
- Excessive bleeding
- Blood clots
- Damage to blood vessels or arteries
- Dislocation (in total hip replacement)
- Limb length inequality (in total hip replacement)
Your doctor will discuss all the possible complications with you before your surgery.
Recovery. How long it takes to recover and resume your daily activities will depend on several factors, including your general health and the type of surgical procedure you have. Initially, you may need a cane, walker, or crutches to walk. Your doctor may recommend physical therapy to help you regain strength in your hip and to restore range of motion.
Outcomes
Inflammatory arthritis of the hip can cause a wide range of disabling symptoms. Today, new medications may prevent progression of disease and joint destruction. Early treatment can help preserve the hip joint.
In cases that progress to severe joint damage, surgery can relieve your pain, increase motion, and help you get back to enjoying everyday activities. Total hip replacement is one of the most successful operations in all of medicine.
A hip strain occurs when one of the muscles supporting the hip joint is stretched beyond its limit or torn. Strains may be mild, moderate, or severe, depending on the extent of the injury. A severe strain can limit your ability to move your hip.
Anyone can experience a hip strain just doing everyday tasks, but strains most often occur during sports activities.
Although many hip strains improve with simple home treatment, severe strains may require physical therapy or other medical treatment.
Description
The large bones that make up the hip joint—the femur (thighbone) and the pelvis—serve as anchors for several muscles. Some of these muscles move across the abdomen or the buttocks (hip flexors, gluteals). Others move down the thigh to the knee (abductors, adductors, quadriceps, hamstrings).

In a hip strain, muscles and tendons may be injured. Tendons are the tough, fibrous tissues that connect muscles to bones. Hip strains frequently occur near the point where the muscle joins the connective tissue of the tendon.
The strain may be a simple stretch in your muscle or tendon, or it may be a partial or complete tear of muscle fibers or of the muscle and tendon combination.
Once the muscle is injured, it becomes vulnerable to reinjury. Repeated strains in muscles about the hip and pelvis may be associated with athletic pubalgia (also called sports hernia). A sports hernia is a strain or tear of any soft tissue (muscle, tendon, ligament) in the lower abdomen or groin area. This condition is discussed in Sports Hernia (Athletic Pubalgia).

Cause
A hip strain can be an acute injury—meaning that it occurs suddenly, such as from a fall or a direct blow during contact sports. Hip strains are also caused by overuse—when the muscle or tendon has slowly become weakened over time by repetitive movements.
Factors that put you at greater risk for a hip strain include:
- Prior injury in the same area
- Muscle tightness
- Failure to warm up properly before exercising
- Attempting to do too much, too quickly, when you exercise
Symptoms
A muscle strain causes pain and tenderness in the injured area. Other symptoms may include:
- Increased pain when you use the muscle
- Swelling
- Limited range of motion
- Muscle weakness
Home Remedies
Many hip strains will improve with simple home treatment. Mild strains can be treated with the RICE protocol. RICE stands for rest, ice, compression, and elevation.
- Rest. Avoid activities that put weight on the hip for the first few days after the injury.
- Ice. Apply ice immediately after the injury to keep the swelling down. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly on the skin.
- Compression. To prevent additional swelling, lightly wrap the area in a soft bandage or wear compression shorts.
- Elevation. As often as possible, rest with your leg raised up higher than your heart.
In addition, non-steroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen and naproxen, can help reduce swelling and relieve pain.
If the pain persists or it becomes more difficult to move your hip and leg, contact your doctor.
Doctor Examination
Physical Examination
Your doctor will discuss your general health and ask you about what activities you were doing just prior to the injury. He or she will examine your leg and hip for tenderness or swelling. During the physical examination, your doctor will apply pressure to various muscles in the area and move your leg and hip in various directions to assess your range of motion.
Your doctor may also ask you to perform a variety of stretches and movements to help determine which muscle is injured.
X-Rays
X-rays provide images of dense structures such as bone. Your doctor may order an x-ray to rule out the possibility of a stress fracture of the hip, which has similar symptoms. In most cases, no additional imaging tests are needed to confirm the diagnosis.
Treatment
Medical treatment for muscle strains is designed to relieve pain and restore range of motion and strength. The majority of hip strains are treated nonsurgically.
Nonsurgical Treatment
In addition to the RICE method and anti-inflammatory medication, your doctor may recommend using crutches for a few days to limit the weight on your hip. Other recommendations may include:
- Heat therapy. Ice should be applied immediately after an acute injury to reduce swelling. After 72 hours, however, alternating ice with heat therapy—which may include soaking in a hot bath or using a heat lamp or heating pad—may help relieve pain and improve range of motion.
- Home exercise program. Specific exercises can strengthen the muscles that support the hip and help to improve muscle endurance and flexibility.
- Physical therapy. If pain persists after a few weeks of home exercise, your doctor may recommend formal physical rehabilitation. A physical therapist can provide an individualized exercise program to improve strength and flexibility.
Surgical Treatment
Severe injuries in which the muscle fibers are completely torn may require surgery in order to return to normal function and movement. Surgery typically involves stitching the torn pieces back together.
Many severe hip strains are successfully treated without surgery. Your doctor will discuss the treatment options that best meet your individual health needs.
Recovery
In most cases, you should avoid the activity that caused your injury for 10 to14 days. A severe muscle strain may require a longer period of recovery. If your pain returns when you resume more strenuous activity, however, discontinue what you are doing and go back to easier activities that do not cause pain.
You can take the following precautions to help prevent muscle strains in the future:
- Condition your muscles with a regular program of exercise. Ask your doctor about exercise programs for people of your age and activity level.
- Warm up before any exercise session or sports activity, including practice. A good warm up prepares your body for more intense activity. It gets your blood flowing, raises your muscle temperature, and increases your breathing rate. Warming up gives your body time to adjust to the demands of exercise. It increases your range of motion and reduces stiffness.
- Wear or use appropriate protective gear for your sport.
- Take time to cool down after exercise. Instead of performing a large number of rapid stretches, stretch slowly and gradually, holding each stretch to give your muscle time to respond and lengthen. You can find examples of stretching exercises in the Related Resources section of this article or ask your doctor or coach for help in developing a routine.
- Take the time needed to let your muscle heal before you return to sports. Wait until your muscle strength and flexibility return to preinjury levels.
Total Hip Replacement
Information on total hip replacement is also available in Spanish: Reemplazo total de cadera and Portuguese: Artroplastia total de quadril.
Whether you have just begun exploring treatment options or have already decided to undergo hip replacement surgery, this information will help you understand the benefits and limitations of total hip replacement. This article describes how a normal hip works, the causes of hip pain, what to expect from hip replacement surgery, and what exercises and activities will help restore your mobility and strength, and enable you to return to everyday activities.
If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking supports do not adequately help your symptoms, you may consider hip replacement surgery. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
First performed in 1960, hip replacement surgery is one of the most successful operations in all of medicine. Since 1960, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement. According to the Agency for Healthcare Research and Quality, more than 300,000 total hip replacements are performed each year in the United States.
Anatomy
The hip is one of the body’s largest joints. It is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
A thin tissue called synovial membrane surrounds the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during hip movement.
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint.

Common Causes of Hip Pain
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
- Osteoarthritis. This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood.
- Rheumatoid arthritis. This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed “inflammatory arthritis.”
- Post-traumatic arthritis. This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time.
- Avascular necrosis. An injury to the hip, such as a dislocation or fracture, may limit the blood supply to the femoral head. This is called avascular necrosis (also commonly referred to as “osteonecrosis”). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause avascular necrosis.
- Childhood hip disease. Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later on in life. This happens because the hip may not grow normally, and the joint surfaces are affected.

Animation courtesy Visual Health Solutions, Inc.
Description
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or “press fit” into the bone.
- A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.

Animation courtesy Visual Health Solutions, Inc.
Is Hip Replacement Surgery for You?
The decision to have hip replacement surgery should be a cooperative one made by you, your family, your primary care doctor, and your orthopaedic surgeon. The process of making this decision typically begins with a referral by your doctor to an orthopaedic surgeon for an initial evaluation.
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total hip replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
When Surgery Is Recommended
There are several reasons why your doctor may recommend hip replacement surgery. People who benefit from hip replacement surgery often have:
- Hip pain that limits everyday activities, such as walking or bending
- Hip pain that continues while resting, either day or night
- Stiffness in a hip that limits the ability to move or lift the leg
- Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
The Orthopaedic Evaluation
An evaluation with an orthopaedic surgeon consists of several components.
- Medical history. Your orthopaedic surgeon will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities.
- Physical examination. This will assess hip mobility, strength, and alignment.
- X-rays. These images help to determine the extent of damage or deformity in your hip.
- Other tests. Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.


Deciding to Have Hip Replacement Surgery
Talk With Your Doctor
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options — such as medications, physical therapy, or other types of surgery — also may be considered.
In addition, your orthopaedic surgeon will explain the potential risks and complications of hip replacement surgery, including those related to the surgery itself and those that can occur over time after your surgery.
Never hesitate to ask your doctor questions when you do not understand. The more you know, the better you will be able to manage the changes that hip replacement surgery will make in your life.
Realistic Expectations
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and cannot do. Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living.
With normal use and activity, the material between the head and the socket of every hip replacement implant begins to wear. Excessive activity or being overweight may speed up this normal wear and cause the hip replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports.
Realistic activities following total hip replacement include unlimited walking, swimming, golf, driving, hiking, biking, dancing, and other low-impact sports.
With appropriate activity modification, hip replacements can last for many years.
Preparing for Surgery
Medical Evaluation
If you decide to have hip replacement surgery, your orthopaedic surgeon may ask you to have a complete physical examination by your primary care doctor before your surgical procedure. This is needed to make sure you are healthy enough to have the surgery and complete the recovery process. Many patients with chronic medical conditions, like heart disease, may also be evaluated by a specialist, such a cardiologist, before the surgery.
Tests
Several tests, such as blood and urine samples, an electrocardiogram (EKG), and chest x-rays, may be needed to help plan your surgery.
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for treatment to improve your skin before surgery.
Blood Donations
You may be advised to donate your own blood prior to surgery. It will be stored in the event you need blood after surgery.
Medications
Tell your orthopaedic surgeon about the medications you are taking. He or she or your primary care doctor will advise you which medications you should stop taking and which you can continue to take before surgery.
Weight Loss
If you are overweight, your doctor may ask you to lose some weight before surgery to minimize the stress on your new hip and possibly decrease the risks of surgery.
Dental Evaluation
Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary Evaluation
Individuals with a history of recent or frequent urinary infections should have a urological evaluation before surgery. Older men with prostate disease should consider completing required treatment before having surgery.
Social Planning
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone, your orthopaedic surgeon’s office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility during your recovery after surgery also may be arranged.
Home Planning
Several modifications can make your home easier to navigate during your recovery. The following items may help with daily activities:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
![fig40 [Converted]](http://st9.idsil.com/dev/doctors/dukeahn/wp-content/uploads/sites/8/2016/12/hip-implants-img6.jpg)
Your Surgery
You will most likely be admitted to the hospital on the day of your surgery.
Anesthesia
After admission, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia are general anesthesia (you are put to sleep) or spinal, epidural, or regional nerve block anesthesia (you are awake but your body is numb from the waist down). The anesthesia team, with your input, will determine which type of anesthesia will be best for you.
Implant Components
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of highly polished strong metal or ceramic material) and the socket component (a durable cup of plastic, ceramic or metal, which may have an outer metal shell).
The prosthetic components may be “press fit” into the bone to allow your bone to grow onto the components or they may be cemented into place. The decision to press fit or to cement the components is based on a number of factors, such as the quality and strength of your bone. A combination of a cemented stem and a non-cemented socket may also be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs.

OLYMPUS DIGITAL CAMERA

OLYMPUS DIGITAL CAMERA
Procedure
The surgical procedure takes a few hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip.

After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room.
Your Stay in the Hospital
You will most likely stay in the hospital for a few days. To protect your hip during early recovery, a positioning splint, such as a foam pillow placed between your legs, may be used.
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Physical Therapy

Home Health – Respiratory Therapy
Walking and light activity are important to your recovery. Most patients who undergo total hip replacement begin standing and walking with the help of a walking support and a physical therapist the day after surgery. In some cases, patients begin standing and walking on the actual day of surgery. The physical therapist will teach you specific exercises to strengthen your hip and restore movement for walking and other normal daily activities.
Preventing Pneumonia
It is common for patients to have shallow breathing in the early postoperative period. This is usually due to the effects of anesthesia, pain medications, and increased time spent in bed. This shallow breathing can lead to a partial collapse of the lungs (termed “atelectasis”) which can make patients susceptible to pneumonia. To help prevent this, it is important to take frequent deep breaths. Your nurse may provide a simple breathing apparatus called a spirometer to encourage you to take deep breaths.
Recovery
The success of your surgery will depend in large measure on how well you follow your orthopaedic surgeon’s instructions regarding home care during the first few weeks after surgery.
Wound Care
You may have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity

Mature woman in physical therapy
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include:
- A graduated walking program to slowly increase your mobility, initially in your home and later outside
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore movement and strengthen your hip. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center the first few weeks after surgery
Possible Complications of Surgery
The complication rate following hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2% of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur they can prolong or limit full recovery.
Infection
Infection may occur superficially in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later.
Minor infections of the wound are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood Clots

Blood clots in the leg veins or pelvis are one of the most common complications of hip replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopaedic surgeon will outline a prevention program which may include blood thinning medications, support hose, inflatable leg coverings, ankle pump exercises, and early mobilization.
Leg-length Inequality
Sometimes after a hip replacement, one leg may feel longer or shorter than the other. Your orthopaedic surgeon will make every effort to make your leg lengths even, but may lengthen or shorten your leg slightly in order to maximize the stability and biomechanics of the hip. Some patients may feel more comfortable with a shoe lift after surgery.
Dislocation
This occurs when the ball comes out of the socket. The risk for dislocation is greatest in the first few months after surgery while the tissues are healing. Dislocation is uncommon. If the ball does come out of the socket, a closed reduction usually can put it back into place without the need for more surgery. In situations in which the hip continues to dislocate, further surgery may be necessary.

Loosening and Implant Wear
Over years, the hip prosthesis may wear out or loosen. This is most often due to everyday activity. It can also result from a biologic thinning of the bone called osteolysis. If loosening is painful, a second surgery called a revision may be necessary.
Other Complications
Nerve and blood vessel injury, bleeding, fracture, and stiffness can occur. In a small number of patients, some pain can continue or new pain can occur after surgery.
Avoiding Problems After Surgery
Recognizing the Signs of a Blood Clot
Follow your orthopaedic surgeon’s instructions carefully to reduce the risk of blood clots developing during the first several weeks of your recovery. He or she may recommend that you continue taking the blood thinning medication you started in the hospital. Notify your doctor immediately if you develop any of the following warning signs.
Warning signs of blood clots. The warning signs of possible blood clot in your leg include:
- Pain in your calf and leg that is unrelated to your incision
- Tenderness or redness of your calf
- New or increasing swelling of your thigh, calf, ankle, or foot
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection
A common cause of infection following hip replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections.
Following surgery, patients with certain risk factors may need to take antibiotics prior to dental work, including dental cleanings, or before any surgical procedure that could allow bacteria to enter your bloodstream. Your orthopaedic surgeon will discuss with you whether taking preventive antibiotics before dental procedures is needed in your situation.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible hip replacement infection:
- Persistent fever (higher than 100°F orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the hip wound
- Drainage from the hip wound
- Increasing hip pain with both activity and rest
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails or have someone help you until you improve your balance, flexibility, and strength.
Your orthopaedic surgeon and physical therapist will help you decide which assistive aides will be required following surgery, and when those aides can safely be discontinued.
Other Precautions
To assure proper recovery and prevent dislocation of the prosthesis, you may be asked to take special precautions when sitting, bending, or sleeping — usually for the first 6 weeks after surgery. These precautions will vary from patient to patient, depending on the surgical approach your surgeon used to perform your hip replacement.
Prior to discharge from the hospital, your surgeon and physical therapist will provide you with any specific precautions you should follow.
Outcomes
How Your New Hip Is Different
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time, and most patients find these are minor compared with the pain and limited function they experienced prior to surgery.
Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask your orthopaedic surgeon for a card confirming that you have an artificial hip.
Protecting Your Hip Replacement
There are many things you can do to protect your hip replacement and extend the life of your hip implant.
- Participate in a regular light exercise program to maintain proper strength and mobility of your new hip.
- Take special precautions to avoid falls and injuries. If you break a bone in your leg, you may require more surgery.
- Make sure your dentist knows that you have a hip replacement. Talk with your orthopaedic surgeon about whether you need to take antibiotics prior to dental procedures.
- See your orthopaedic surgeon periodically for routine follow-up examinations and x-rays, even if your hip replacement seems to be doing fine.
Arthritis literally means “inflammation of a joint.” In some forms of arthritis, such as osteoarthritis, the inflammation arises because the smooth covering (articular cartilage) on the ends of bones become damaged or worn. Osteoarthritis is usually found in one, usually weightbearing, joint.
In other forms of arthritis, such as rheumatoid arthritis, the joint lining becomes inflamed as part of a disease process that affects the entire body. Some other types of arthritis are: seronegative spondyloarthropathies, crytalline deposition diseases, and septic arthritis.
Arthritis is a major cause of lost work time and serious disability for many people. Although arthritis is mainly a disease of adults, children may also have it.
Anatomy
Arthritis is a disease of the joint. A joint is where the ends of two or more bones meet. The knee joint, for example, is formed between the bones of the lower leg (the tibia and the fibula) and the thighbone (the femur). The hip joint is where the top of the thighbone (femoral head) meets a concave portion of the pelvis (the acetabulum).
A smooth tissue of cartilage covers the ends of bones in a joint. Cartilage cushions the bone and allows the joint to move easily without the friction that would come with bone-on-bone contact. A joint is enclosed by a fibrous envelope, called the synovium, which produces a fluid that also helps to reduce friction and wear in a joint. Ligaments connect the bones and keep the joint stable. Muscles and tendons power the joint and enable it to move.
Cause
There are two major categories of arthritis.

The first type is caused by wear and tear on the articular cartilage (osteoarthritis) through the natural aging process, through constant use, or through trauma (post-traumatic arthritis).
The second type is caused by one of a number of inflammatory processes.
Regardless of whether the cause is from injury, normal wear and tear, or disease, the joint becomes inflamed, causing swelling, pain and stiffness. This is usually temporary. Inflammation is one of the body’s normal reactions to injury or disease. In arthritic joints, however, inflammation may cause long-lasting or permanent disability.
Natural History
Osteoarthritis

The most common type of arthritis is osteoarthritis. It results from overuse, trauma, or the degeneration of the joint cartilage that takes place with age. Osteoarthritis is often more painful in joints that bear weight, such as the knee, hip, and spine, rather than in the wrist, elbow, and shoulder joints. However, joints that are used extensively in work or sports or joints that have been damaged from fractures or other injuries may show signs of osteoarthritis. Other disorders that injure or overload the articular cartilage may lead to osteoarthritis.
In osteoarthritis, the cartilage covering the bone ends gradually wears away. In many cases, bone growths called “spurs” develop at the edges of osteoarthritic joints. The bone can become hard and firm (sclerosis). The joint becomes inflamed, causing pain and swelling. Continued use of the joint
Rheumatoid Arthritis

Rheumatoid arthritis is a long-lasting disease. It is estimated that 1% of the population throughout the world have rheumatoid arthritis. Women are three times more likely than men to have rheumatoid arthritis. The development of rheumatoid arthritis slows with age.
Rheumatoid arthritis affects many parts of the body, but mainly the joints. The body’s immune system, which normally protects the body, begins to produce substances that attack the body. In rheumatoid arthritis, the joint lining swells, invading surrounding tissues. Chemical substances are produced that attack and destroy the joint surface.
Rheumatoid arthritis may affect both large and small joints in the body and also the spine. Swelling, pain, and stiffness usually develop, even when the joint is not used. In some circumstances, juvenile arthritis may cause similar symptoms in children.
Diagnosis
Arthritis is diagnosed through a careful evaluation of symptoms and a physical examination. X-rays are important to show the extent of any damage to the joint. Blood tests and other laboratory tests may help to determine the type of arthritis. Some of the findings of arthritis include:
- Weakness (atrophy) in the muscles
- Tenderness to touch
- Limited ability to move the joint passively (with assistance) and actively (without assistance).
- Signs that other joints are painful or swollen (an indication of rheumatoid arthritis)
- A grating feeling or sound (crepitus) with movement
- Pain when pressure is placed on the joint or the joint is moved
Medications
Over-the-counter medications can be used to control pain and inflammation in the joints. These medications, called anti-inflammatory drugs, include aspirin, ibuprofen, and naproxen. Acetaminophen can be effective in controlling pain.
Prescription medications also are available. A physician will choose a medication by taking into account the type of arthritis, its severity, and the patient’s general physical health. Patients with ulcers, asthma, kidney, or liver disease, for example, may not be able to safely take anti-inflammatory medications.
Injections of cortisone into the joint may temporarily help to relieve pain and swelling. It is important to know that repeated, frequent injections into the same joint can damage it, causing undesirable side effects.
Viscosupplementation or injection of hyaluronic acid preparations can also be helpful in lubricating the joint. This is typically perfomed in the knee.
Exercise and Therapy

Canes, crutches, walkers, or splints may help relieve the stress and strain on arthritic joints. Learning methods of performing daily activities that are the less stressful to painful joints also may be helpful.
Certain exercises and physical therapy may be used to decrease stiffness and to strengthen the weakened muscles around the joint.
Surgery
In general, an orthopaedic surgeon will perform surgery for arthritis when other methods of nonsurgical treatment have failed to relieve pain and other symptoms. When deciding on the type of surgery, the physician and patient will take into account the type of arthritis, its severity, and the patient’s physical condition.
There are a number of surgical procedures. These include:
- Removing the diseased or damaged joint lining
- Realignment of the joints
- Fusing the ends of the bones in the joint together, to prevent joint motion and relieve joint pain
- Replacing the entire joint (total joint replacement)
Long-Term Management

In most cases, persons with arthritis can continue to perform normal activities of daily living. Exercise programs, anti-inflammatory drugs, and weight reduction for obese persons are common measures to reduce pain, stiffness, and improve function.
In persons with severe cases of arthritis, orthopaedic surgery can often provide dramatic pain relief and restore lost joint function.
Some types of arthritis, such as rheumatoid arthritis, are often treated by a team of health care professionals. These professionals may include rheumatologists, physical and occupational therapists, social workers, rehabilitation specialists, and orthopaedic surgeons.
Research
At present, most types of arthritis cannot be cured. Researchers continue to make progress in finding the underlying causes for the major types of arthritis. In the meantime, orthopaedic surgeons, working with other physicians and scientists, have developed many effective treatments for arthritis.
Hip Fractures
A hip fracture is a break in the upper quarter of the femur (thigh) bone. The extent of the break depends on the forces that are involved. The type of surgery used to treat a hip fracture is primarily based on the bones and soft tissues affected or on the level of the fracture.
Anatomy
The “hip” is a ball-and-socket joint. It allows the upper leg to bend and rotate at the pelvis. An injury to the socket, or acetabulum, itself is not considered a “hip fracture.” Management of fractures to the socket is a completely different consideration.

Causes
Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting.
Symptoms
The patient with a hip fracture will have pain over the outer upper thigh or in the groin. There will be significant discomfort with any attempt to flex or rotate the hip.
If the bone has been weakened by disease (such as a stress injury or cancer), the patient may notice aching in the groin or thigh area for a period of time before the break. If the bone is completely broken, the leg may appear to be shorter than the noninjured leg. The patient will often hold the injured leg in a still position with the foot and knee turned outward (external rotation).
Doctor Examination
Imaging
The diagnosis of a hip fracture is generally made by an X-ray of the hip and femur.

In some cases, if the patient falls and complains of hip pain, an incomplete fracture may not be seen on a regular X-ray. In that case, magnetic resonance imaging (MRI) may be recommended. The MRI scan will usually show a hidden fracture.

If the patient is unable to have an MRI scan because of an associated medical condition, computed tomography (CT) may be obtained instead. Computed tomography, however, is not as sensitive as MRI for seeing hidden hip fractures.
Types of Fractures
In general, there are three different types of hip fractures. The type of fracture depends on what area of the upper femur is involved.
Intracapsular Fracture
These fractures occur at the level of the neck and the head of the femur, and are generally within the capsule. The capsule is the soft-tissue envelope that contains the lubricating and nourishing fluid of the hip joint itself.

Intertrochanteric Fracture
This fracture occurs between the neck of the femur and a lower bony prominence called the lesser trochanter. The lesser trochanter is an attachment point for one of the major muscles of the hip. Intertrochanteric fractures generally cross in the area between the lesser trochanter and the greater trochanter. The greater trochanter is the bump you can feel under the skin on the outside of the hip. It acts as another muscle attachment point.

Subtrochanteric Fracture
This fracture occurs below the lesser trochanter, in a region that is between the lesser trochanter and an area approximately 2 1/2 inches below .

In more complicated cases, the amount of breakage of the bone can involve more than one of these zones. This is taken into consideration when surgical repair is considered.
Treatment
Considerations
Once the diagnosis of the hip fracture has been made, the patient’s overall health and medical condition will be evaluated. In very rare cases, the patient may be so ill that surgery would not be recommended. In these cases, the patient’s overall comfort and level of pain must be weighed against the risks of anesthesia and surgery.
Most surgeons agree that patients do better if they are operated on fairly quickly. It is, however, important to insure patients’ safety and maximize their overall medical health before surgery. This may mean taking time to do cardiac and other diagnostic studies.
Nonsurgical Treatment
Patients who might be considered for nonsurgical treatment include those who are too ill to undergo any form of anesthesia and people who were unable to walk before their injury and may have been confined to a bed or a wheelchair.
Certain types of fractures may be considered stable enough to be managed with nonsurgical treatment. Because there is some risk that these “stable” fractures may instead prove unstable and displace (change position), the doctor will need to follow with periodic X-rays of the area. If patients are confined to bed rest as part of the management for these fractures, they will need to be closely monitored for complications that can occur from prolonged immobilization. These include infections, bed sores, pneumonia, the formation of blood clots, and nutritional wasting.

Surgical Treatment
Before Surgery
Anesthesia for surgery could be either general anesthesia with a breathing tube or spinal anesthesia. In very rare circumstances, where only a few screws are planned for fixation, local anesthesia with heavy sedation can be considered. All patients will receive antibiotics during surgery and for the 24-hours afterward.
Appropriate blood tests, chest X-rays, electrocardiograms, and urine samples will be obtained before surgery. Many elderly patients may have undiagnosed urinary tract infections that could lead to an infection of the hip after surgery.
The surgeon’s decision as to how to best fix a fracture will be based on the area of the hip that is broken and the surgeon’s familiarity with the different systems that are available to manage these injuries.
Intracapsular Fracture
If the head of the femur (“ball”) alone is broken, management will be aimed at fixing the cartilage on the ball that has been injured or displaced. Frequently with these injuries, the socket, or acetabulum, may also be broken. The surgeon will need to take this into consideration as well.
These injuries may be approached either from either the front or back of the hip. In some cases, both approaches are required in order to clearly see and fix the injured bone.
For true intracapsular hip fractures, the surgeon may decide either to fix the fracture with individual screws (percutaneous pinning) or a single larger screw that slides within the barrel of a plate. This compression hip screw will allow the fracture to become more stable by having the broken area impact on itself. Occasionally, a secondary screw may be added for stability.


If the intracapsular hip fracture is displaced in a younger patient, a surgical attempt will be made to reduce, or realign, the fracture through a larger incision. The fracture will be held together with either individual screws or with the larger compression hip screw.
In these cases, the blood supply to the ball, or head of the femur, may have been damaged at the time of injury (avascular necrosis). Even though the fracture is realigned and fixed into place, the cartilage and underlying supporting bone may not receive adequate blood. Over a period of time, this may cause the femoral head to flatten out. When this occurs, the joint surface becomes irregular. Ultimately, the hip joint may develop a painful arthritis, despite the surgical repair.

In the older patient, the chance that the head of the femur is damaged in this way is higher. It is generally felt that for these displaced fractures, patients will do better if some of the components of the hip are replaced. In some cases, this can mean a replacement of the ball, or head of the femur (hemiarthroplasty). In other cases, this can mean the replacement of both the ball and socket, or head of the femur and acetabulum (total hip replacement).


Intertrochanteric Fracture
Most intertrochanteric fractures are managed with either a compression hip screw or an intramedullary nail, which also allows for impaction at the fracture site.
The compression hip screw is fixed to the outer side of the bone with bone screws and has a large secondary screw (lag screw) that is placed through the plate into the neck and head of the hip (see compression hip screw figure above). The design of the device allows for impaction and compression at the fracture site. This may increase the stability of the area and promote healing.
The intramedullary nail is placed directly into the marrow canal of the bone through an opening made at the top of the greater trochanter. A lag screw is then placed through the nail and up into the neck and head of the hip. As with the compression hip screw, sliding of the lag screw and impaction of the fracture take place.

There are no definitive studies to show that one device is superior to another. The decision as to which to use is based on the surgeon’s preference and experience.
Subtrochanteric Fracture
At the subtrochanteric level, most fractures are managed with a long intramedullary nail together with a large lag screw or they are managed with screws that capture the neck and head of the femur or the area immediately underneath it, if it has remained intact.


In order to keep the bones from rotating around the nail or from shortening (“telescoping”) on the nail, additional screws may be placed at the lower end of the nail in the area of the knee. These are called interlocking screws.
In certain cases, the surgeon may choose to use a plate rather than a nail. The plate will have screws that go into the bone from the lateral, or outer, side of the femur. A single large screw goes into the neck and the head of the femur and appears similar to the compression hip screw, but at a different angle. Secondary screws are then placed through the plate into the bone to hold the fracture in place.

Recovery
Patients may be discharged from the hospital to their home or find that a stay in a rehabilitation facility is necessary to assist them in regaining their ability to walk.
Pain Management
Pain after an injury or surgery is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover faster.
Medications are often prescribed for short-term pain relief after surgery or an injury. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your treatment.
Rehabilitation
Patients may be encouraged to get out of bed on the day following surgery with the assistance of a physical therapist. The amount of weight that is allowed to be placed on the injured leg will be determined by the surgeon and is generally a function of the type of fracture and repair (fixation).
The physical therapist will work with the patient to help regain strength and the ability to walk. This process may take up to three months.
Medical Care
Occasionally, a blood transfusion may be required after surgery, but longer term antibiotics are generally not necessary.
Most patients will be placed on medicine to thin their blood to reduce the chances of developing blood clots for up to 6 weeks. These medicines may be in the form of pills or injections. Elastic compression stockings or inflatable compression boots may also be used.
Follow-Up Care
During the appointments that take place after surgery, the surgeon will want to check the wound, remove sutures, follow the healing process using X-rays, and prescribe additional physical therapy, if necessary.
Following hip fracture surgery, most patients will regain much, if not all, of the mobility and independence they had before the injury.
For More Information
If you found this article helpful, you may also be interested in Fractures (Broken Bones).
In order to assist doctors in the management of hip fractures in the elderly, the American Academy of Orthopaedic Surgeons has done research to provide some useful guidelines. These are recommendations only and may not apply to each and every individual case. For more information: AAOS Clinical Practice Guideline: Management of Hip Fractures in the Elderly.
![]()
Co-developed by the Orthopaedic Trauma Association
This article addresses hip dislocation that results from a traumatic injury. To learn about pediatric developmental hip dislocation, please read Developmental Dislocation (Dysplasia) of the Hip (DDH). To learn about dislocation after total hip replacement, please read Total Hip Replacement.
A traumatic hip dislocation occurs when the head of the thighbone (femur) is forced out of its socket in the hip bone (pelvis). It typically takes a major force to dislocate the hip. Car collisions and falls from significant heights are common causes and, as a result, other injuries like broken bones often occur with the dislocation.
A hip dislocation is a serious medical emergency. Immediate treatment is necessary.
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A smooth tissue called articular cartilage covers the surface of the ball and the socket. It creates a low friction surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket, creating a tight seal and helping to provide stability to the joint.

Description
When there is a hip dislocation, the femoral head is pushed either backward out of the socket, or forward.
- Posterior dislocation. In approximately 90% of hip dislocation patients, the thighbone is pushed out of the socket in a backwards direction. This is called a posterior dislocation. A posterior dislocation leaves the lower leg in a fixed position, with the knee and foot rotated in toward the middle of the body.
- Anterior dislocation. When the thighbone slips out of its socket in a forward direction, the hip will be bent only slightly, and the leg will rotate out and away from the middle of the body.
When the hip dislocates, the ligaments, labrum, muscles, and other soft tissues holding the bones in place are often damaged, as well. The nerves around the hip may also be injured.
Symptoms
A hip dislocation is very painful. Patients are unable to move the leg and, if there is nerve damage, may not have any feeling in the foot or ankle area.
Cause
Motor vehicle collisions are the most common cause of traumatic hip dislocations. The dislocation often occurs when the knee hits the dashboard in a collision. This force drives the thigh backwards, which drives the ball head of the femur out of the hip socket. Wearing a seatbelt can greatly reduce your risk of hip dislocation during a collision.
A fall from a significant height (such as from a ladder) or an industrial accident can also generate enough force to dislocate a hip.
With hip dislocations, there are often other related injuries, such as fractures in the pelvis and legs, and back, abdominal, knee, and head injuries. Perhaps the most common fracture occurs when the head of the femur hits and breaks off the back part of the hip socket during the injury. This is called a posterior wall acetabular fracture-dislocation.
Doctor Examination
A hip dislocation is a medical emergency. Call for help immediately. Do not try to move the injured person, but keep him or her warm with blankets.
In cases in which hip dislocation is the only injury, an orthopaedic surgeon can often diagnose it simply by looking at the position of the leg. Because hip dislocations often occur with additional injuries, your doctor will complete a thorough physical evaluation.
Your doctor may order imaging tests, such as x-rays, to show the exact position of the dislocated bones, as well as any additional fractures in the hip or thighbone.
Treatment
Reduction Procedures
If there are no other injuries, the doctor will administer an anesthetic or a sedative and manipulate the bones back into their proper position. This is called a reduction.
In some cases, the reduction must be done in the operating room with anesthesia. In rare cases, torn soft tissues or small bony fragments block the bone from going back into the socket. When this occurs, surgery is required to remove the loose tissues and correctly position the bones.
Following reduction, the surgeon will request another set of x-rays and possibly a computed tomography (CT) scan to make sure that the bones are in the proper position.


Complications
A hip dislocation can have long-term consequences, particularly if there are associated fractures.
- Nerve injury. As the thighbone is pushed out of the socket, particularly in posterior dislocations, it can crush and stretch nerves in the hip. The sciatic nerve, which extends from the lower back down the back of the legs, is the nerve most commonly affected. Injury to the sciatic nerve may cause weakness in the lower leg and affect the ability to move the knee, ankle and foot normally. Sciatic nerve injury occurs in approximately 10% of hip dislocation patients. The majority of these patients will experience some nerve recovery.
- Osteonecrosis. As the thighbone is pushed out of the socket, it can tear blood vessels and nerves. When blood supply to the bone is lost, the bone can die, resulting in osteonecrosis (also called avascular necrosis). This is a painful condition that can ultimately lead to the destruction of the hip joint and arthritis.
- Arthritis. The protective cartilage covering the bone may also be damaged, which increases the risk of developing arthritis in the joint. Arthritis can eventually lead to the need for other procedures, like a total hip replacement.
Recovery
It takes time—sometimes 2 to 3 months—for the hip to heal after a dislocation. The rehabilitation time may be longer if there are additional fractures. The doctor may recommend limiting hip motion for several weeks to protect the hip from dislocating again. Physical therapy is often recommended during recovery.
Patients often begin walking with crutches within a short time. Walking aids, such as walkers, crutches and, eventually, canes, help patients get mobilized.
This article is also available in Spanish: Bursitis de cadera (Hip Bursitis).
Bursae, are small, jelly-like sacs that are located throughout the body, including around the shoulder, elbow, hip, knee, and heel. They contain a small amount of fluid, and are positioned between bones and soft tissues, acting as cushions to help reduce friction.
Bursitis is inflammation of the bursa. There are two major bursae in the hip that typically become irritated and inflamed. One bursa covers the bony point of the hip bone called the greater trochanter. Inflammation of this bursa is called trochanteric bursitis.
Another bursa — the iliopsoas bursa — is located on the inside (groin side) of the hip. When this bursa becomes inflamed, the condition is also sometimes referred to as hip bursitis, but the pain is located in the groin area. This condition is not as common as trochanteric bursitis, but is treated in a similar manner.

Symptoms
The main symptom of trochanteric bursitis is pain at the point of the hip. The pain usually extends to the outside of the thigh area. In the early stages, the pain is usually described as sharp and intense. Later, the pain may become more of an ache and spread across a larger area of the hip.
Typically, the pain is worse at night, when lying on the affected hip, and when getting up from a chair after being seated for a while. It also may get worse with prolonged walking, stair climbing, or squatting.
Risk Factors
Hip bursitis can affect anyone, but is more common in women and middle-aged or elderly people. It is less common in younger people and in men.
The following risk factors have been associated with the development of hip bursitis.
- Repetitive stress (overuse) injury. This can occur when running, stair climbing, bicycling, or standing for long periods of time.
- Hip injury. An injury to the point of your hip can occur when you fall onto your hip, bump your hip, or lie on one side of your body for an extended period of time.
- Spine disease. This includes scoliosis, arthritis of the lumbar (lower) spine, and other spine problems.
- Leg-length inequality. When one leg is significantly shorter than the other, it affects the way you walk, and can lead to irritation of a hip bursa.
- Rheumatoid arthritis. This makes the bursa more likely to become inflamed.
- Previous surgery. Surgery around the hip or prosthetic implants in the hip can irritate the bursa and cause bursitis.
- Bone spurs or calcium deposits. These can develop within the tendons that attach muscles to the trochanter. They can irritate the bursa and cause inflammation.
Doctor Examination
To diagnose hip bursitis, the doctor will perform a comprehensive physical examination, looking for tenderness in the area of the point of the hip. He or she may also perform additional tests to rule out other possible injuries or conditions. These tests can include imaging studies, such as x-rays, bone scanning, and magnetic resonance imaging (MRI).
Treatment
Nonsurgical Treatment
The initial treatment for hip bursitis does not involve surgery. Many people with hip bursitis can experience relief with simple lifestyle changes, including:
- Activity modification. Avoid the activities that worsen symptoms.
- Non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen, naproxen, piroxicam, celecoxib, and others, may relieve pain and control inflammation.Use NSAIDs cautiously and for limited periods. Talk with your doctor about the NSAIDs you use. NSAIDs may have adverse side effects if you have certain medical conditions or take certain medications.
- Assistive devices. Use of a walking cane or crutches for a week or more when needed.
- Physical therapy. Your doctor may prescribe exercises to increase hip strength and flexibility. You may do these exercises on your own, or a physical therapist may teach you how to stretch your hip muscles and use other treatments such as rolling therapy (massage), ice, heat, or ultrasound.
- Steroid injection. Injection of a corticosteroid along with a local anesthetic may also be helpful in relieving symptoms of hip bursitis. This is a simple and effective treatment that can be done in the doctor’s office. It involves a single injection into the bursa. The injection may provide temporary (months) or permanent relief. If pain and inflammation return, another injection or two, given a few months apart, may be needed. It is important to limit the number of injections, as prolonged corticosteroid injections may damage the surrounding tissues.
Surgical Treatment
Surgery is rarely needed for hip bursitis. If the bursa remains inflamed and painful after all nonsurgical treatments have been tried, your doctor may recommend surgical removal of the bursa. Removal of the bursa does not hurt the hip, and the hip can function normally without it.
A newer technique that is gaining popularity is arthroscopic removal of the bursa. In this technique, the bursa is removed through a small (1/4-inch) incision over the hip. A small camera, or arthroscope, is placed in a second incision so the doctor can guide miniature surgical instruments and cut out the bursa. This surgery is less invasive, and recovery is quicker and less painful.
Both types of surgeries are done on an outpatient (same-day) basis, so an overnight stay in the hospital is not usually necessary. Early studies show arthroscopic removal of the bursa to be quite effective, but this is still being studied.
Rehabilitation
Following surgery, a short rehabilitation period can be expected. Most patients find that using a cane or crutches for a couple of days is helpful. It is reasonable to be up and walking around the evening after surgery. The soreness from surgery usually goes away after a few days.
Prevention
Although hip bursitis cannot always be prevented, there are things you can do to prevent the inflammation from getting worse.
- Avoid repetitive activities that put stress on the hips.
- Lose weight if you need to.
- Get a properly fitting shoe insert for leg-length differences.
- Maintain strength and flexibility of the hip muscles.
If you found this article helpful, you may also be interested in What Are NSAIDs?.
Pelvic Fractures
The pelvis is the sturdy ring of bones located at the base of the spine. Fractures of the pelvis are uncommon—accounting for only about 3% of all adult fractures.
Most pelvic fractures are caused by some type of traumatic, high-energy event, such as a car collision. Because the pelvis is in proximity to major blood vessels and organs, pelvic fractures may cause extensive bleeding and other injuries that require urgent treatment.
In some cases, a lower-impact event—such as a minor fall—may be enough to cause a pelvic fracture in an older person who has weaker bones.
Treatment for a pelvic fracture varies depending on the severity of the injury. While lower-energy fractures can often be managed with conservative care, treatment for high-energy pelvic fractures usually involves surgery to reconstruct the pelvis and restore stability so that patients can resume their daily activities.
The pelvis is a ring of bones located at the lower end of the trunk—between the spine and the legs. The pelvic bones include the:
- Sacrum (the large triangular bone at the base of the spine)
- Coccyx (tailbone)
- Hip bones
Each hip bone contains three bones—the ilium, ischium, and pubis—that are separate during childhood but fuse together as we grow older. These three bones meet to form the acetabulum—the hollow cup that serves as the socket for the ball-and-socket hip joint.
Bands of strong connective tissues called ligaments join the pelvis to the sacrum, creating a bowl-like cavity below the rib cage.
Major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs all pass through the pelvic ring. The pelvis protects these important structures from injury. It also serves as an anchor for the muscles of the hip, thigh, and abdomen.

Because the pelvis is a ring-like structure, a fracture in one part of the structure is often accompanied by a fracture or damage to ligaments at another point in the structure. Doctors have identified several common pelvic fracture patterns. The specific pattern of the fracture depends upon the direction in which it was broken and the amount of force that caused the injury.
In addition to being described by the specific fracture pattern, pelvic fractures are often described as “stable” or “unstable,” based on how much damage has occurred to the structural integrity of the pelvic ring.
Stable fracture. In this type of fracture, there is often only one break in the pelvic ring and the broken ends of the bones line up adequately. Low-energy fractures are often stable fractures. Stable pelvic fracture patterns include:



Unstable fracture. In this type of fracture, there are usually two or more breaks in the pelvic ring and the ends of the broken bones do not line up correctly (displacement). This type of fracture is more likely to occur due to a high-energy event. Unstable pelvic fracture patterns include:



Both stable and unstable pelvic fractures can also be divided into “open” fractures, in which the bone fragments stick out through the skin, or “closed” fractures, in which the skin is not broken. Open fractures are particularly serious because, once the skin is broken, infection in both the wound and the bone can occur. Immediate treatment is required to prevent infection.
Cause
High-Energy Trauma
A pelvic fracture may result from a high-energy force, such as that generated during a:
- Car or motorcycle collision
- Crush accident
- Fall from a significant height (such as a ladder)
Depending on the direction and magnitude of the force, these injuries can be life-threatening and require surgical treatment.
Bone Insufficiency
A pelvic fracture may also occur due to weak or insufficient bone. This is most common in older people whose bones have become weakened by osteoporosis. In these patients, a fracture may occur even during a fall from standing or a routine activity such as getting out of the bathtub or descending stairs. These injuries are typically stable fractures that do not damage the structural integrity of the pelvic ring, but may fracture an individual bone.
Other Causes
Less commonly, a fracture may occur when a piece of the ischium bone tears away from the site where the hamstring muscles attach to the bone. This type of fracture is called an avulsion fracture and it is most common in young athletes who are still growing. An avulsion fracture does not usually make the pelvis unstable or injure internal organs.
Symptoms
A fractured pelvis is almost always painful. This pain is aggravated by moving the hip or attempting to walk. Often, the patient will try to keep his or her hip or knee bent in a specific position to avoid aggravating the pain. Some patients may experience swelling or bruising in the hip area.
Doctor Examination
Emergency Stabilization
Patients with high-energy fractures will almost always go or be brought to an urgent care center or emergency room for initial treatment due to the severity of their symptoms.
These patients may also have additional injuries to the head, chest, abdomen, or legs. If their injuries cause significant blood loss, it could lead to shock—a life-threatening condition that can result in organ failure.
The care of patients with high-energy pelvic fractures requires a multidisciplinary approach with input from a number of medical specialists. In some cases, doctors must address airway, breathing, and circulatory problems before treating the fracture and other injuries.
Physical Examination
Your doctor will carefully examine your pelvis, hips, and legs. He or she will also check for nerve injury by assessing whether you can move your ankles and toes and feel sensation on the bottom of your feet.
Your doctor will also carefully examine the rest of your body to determine if you have sustained any other injuries.
Imaging Studies
X-rays. These studies provide images of dense structures, such as bones. All pelvic fractures require x-rays—usually from a number of different angles—to help the doctor determine how displaced place the bones are.

Computed tomography (CT) scans. Because of the complexity of this type of injury, a CT scan is commonly ordered for pelvic fractures. A CT scan will provide a more detailed, cross-sectional image of the pelvis. Your doctor will use this information to better determine the specific pattern and extent of your injury, look for associated injuries, and aid in preoperative planning.
Magnetic resonance imaging (MRI) scans: In rare cases, your doctor may order an MRI scan to discover a fracture that cannot be seen on x-ray or CT scan.
Treatment
Treatment is based on a number of factors, including:
- The specific pattern of the fracture
- How much the bones are displaced
- Your overall condition and associated injuries
Nonsurgical Treatment
Your doctor may recommend nonsurgical treatment for stable fractures in which the bones are nondisplaced or minimally displaced.
Nonsurgical treatments may include:
Walking aids. To avoid bearing weight on your leg, your doctor may recommend that you use crutches or a walker for up to three months—or until your bones are fully healed. If you have injuries above both legs, you may need to use a wheelchair for a period of time so that you can avoid bearing weight on either leg.
Medications. Your doctor may prescribe medication to relieve pain, as well as an anti-coagulant, or blood thinner, to reduce the risk of blood clots forming in the veins of your legs and pelvis.
Surgical Treatment
Patients with unstable pelvic fractures may require one or more surgical procedures.
External fixation. Your doctor may use external fixation to stabilize your pelvic area. In this operation, metal pins or screws are inserted into the bones through small incisions into the skin and muscle. The pins and screws project out of the skin on both sides of the pelvis where they are attached to carbon fiber bars outside the skin. The external fixator acts as a stabilizing frame to hold the broken bones in proper position.
In some cases, an external fixator is used to stabilize the bones until healing is complete. In patients who are unable to tolerate a lengthy, more complicated procedure, an external fixator may be used as a temporary treatment until another procedure can be performed.

Skeletal traction. Skeletal traction is a pulley system of weights and counterweights that helps realign the pieces of bone. Skeletal traction is often used immediately after an injury and removed after surgery. Occasionally, acetabular fractures can be treated with skeletal traction alone. This is rare, however, and will be a decision made jointly with input from your doctor.
During skeletal traction, metal pins are implanted in the thighbone or shinbone to help position the leg. Weights attached to the pins gently pull on the leg, keeping the broken bone fragments in as normal a position as possible. For many patients, skeletal traction also provides some pain relief.
Open reduction and internal fixation. During this operation, the displaced bone fragments are first repositioned (reduced) into their normal alignment. They are then held together with screws or metal plates attached to the outer surface of the bone.

Complications
There are risks associated with any surgical procedure. Before your surgery, your doctor will discuss each of these risks with you and will take specific measures to help avoid potential complications.
Possible complications include:
- Wound healing problems, including infection
- Damage to nerves or blood vessels
- Blood clots
- Pulmonary embolism—a blood clot in the lungs
Recovery
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Early Movement
In most cases, your doctor will encourage early movement. Most patients begin walking—with weight-bearing restrictions—and performing foot and leg exercises as soon as possible after surgery.
Physical Therapy
Specific exercises will help you regain flexibility and restore range of motion in your hip. Other exercises will help you build strength and endurance so that you are better able to perform your daily activities.
Blood Clot Prevention
Although early movement is encouraged, your mobility after surgery will still be somewhat limited. For this reason, your doctor may prescribe an anticoagulant, or blood thinner, to help prevent blood clots from forming in the deep veins of your pelvis and legs.
Weight Bearing
Your doctor may recommend that you use crutches or a walker for a period of time. Full weight bearing is usually allowed by 3 months—or when your bones are fully healed. You may require the use of a cane or walking aid for a longer period of time.
Outcomes
Stable pelvic fractures tend to heal well. Unstable pelvic fractures sustained during high-energy incidents, such as car accidents, may result in significant complications, including severe bleeding, internal organ damage, and infection. If these injuries are addressed successfully, the fracture usually heals well.
You may walk with a limp for several months if damage has occurred to the muscles around your pelvis. These muscles may take up to one year to become strong again.
Subsequent problems, such as pain, impaired mobility, and sexual dysfunction, may result from damage to nerves and organs that is associated with the pelvic fracture.
If you found this article helpful, you may also be interested in Deep Vein Thrombosis.
The hip is a “ball-and-socket” joint. In a normal hip, the ball at the upper end of the thighbone (femur) fits firmly into the socket, which is part of the large pelvis bone. In babies and children with developmental dysplasia (dislocation) of the hip (DDH), the hip joint has not formed normally. The ball is loose in the socket and may be easy to dislocate.
Although DDH is most often present at birth, it may also develop during a child’s first year of life. Recent research shows that babies whose legs are swaddled tightly with the hips and knees straight are at a notably higher risk for developing DDH after birth. As swaddling becomes increasingly popular, it is important for parents to learn how to swaddle their infants safely, and to understand that when done improperly, swaddling may lead to problems like DDH.
In all cases of DDH, the socket (acetabulum) is shallow, meaning that the ball of the thighbone (femur) cannot firmly fit into the socket. Sometimes, the ligaments that help to hold the joint in place are stretched. The degree of hip looseness, or instability, varies among children with DDH.
- Dislocated. In the most severe cases of DDH, the head of the femur is completely out of the socket.
- Dislocatable. In these cases, the head of the femur lies within the acetabulum, but can easily be pushed out of the socket during a physical examination.
- Subluxatable. In mild cases of DDH, the head of the femur is simply loose in the socket. During a physical examination, the bone can be moved within the socket, but it will not dislocate.

In the United States, approximately 1 to 2 babies per 1,000 are born with DDH. Pediatricians screen for DDH at a newborn’s first examination and at every well-baby checkup thereafter.
Cause
DDH tends to run in families. It can be present in either hip and in any individual. It usually affects the left hip and is predominant in:
- Girls
- First-born children
- Babies born in the breech position (especially with feet up by the shoulders). The American Academy of Pediatrics now recommends ultrasound DDH screening of all female breech babies.
- Family history of DDH (parents or siblings)
- Oligohydraminos (low levels of amniotic fluid)
Symptoms
Some babies born with a dislocated hip will show no outward signs.
Contact your pediatrician if your baby has:
- Legs of different lengths
- Uneven skin folds on the thigh
- Less mobility or flexibility on one side
- Limping, toe walking, or a waddling, duck-like gait
Doctor Examination
In addition to visual clues, your doctor will perform a careful physical examination to check for DDH, such as listening and feeling for “clunks” as the hip is put in different positions. Your doctor will use specific maneuvers to determine if the hip can be dislocated and/or put back into proper position.
Newborns identified as at higher risk for DDH are often tested using ultrasound, which can create images of the hip bones. For older infants and children, x-rays of the hip may be taken to provide detailed pictures of the hip joint.
Treatment
When DDH is detected at birth, it can usually be corrected with the use of a harness or brace. If the hip is not dislocated at birth, the condition may not be noticed until the child begins walking. At this time, treatment is more complicated, with less predictable results.
Nonsurgical Treatment
Treatment methods depend on a child’s age.
- Newborns. The baby is placed in a soft positioning device, called a Pavlik harness, for 1 to 2 months to keep the thighbone in the socket. This special brace is designed to hold the hip in the proper position while allowing free movement of the legs and easy diaper care. The Pavlik harness helps tighten the ligaments around the hip joint and promotes normal hip socket formation.
Parents play an essential role in ensuring the harness is effective. Your doctor and healthcare team will teach you how to safely perform daily care tasks, such as diapering, bathing, feeding, and dressing.

- 1 month to 6 months. Similar to newborn treatment, a baby’s thighbone is repositioned in the socket using a harness or similar device. This method is usually successful, even with hips that are initially dislocated.
How long the baby will require the harness varies. It is usually worn full-time for at least 6 weeks, and then part-time for an additional 6 weeks.
If the hip will not stay in position using a harness, your doctor may try an abduction brace made of firmer material that will keep your baby’s legs in position.
In some cases, a closed reduction procedure is required. Your doctor will gently move your baby’s thighbone into proper position, and then apply a body cast (spica cast) to hold the bones in place. This procedure is done while the baby is under anesthesia.
Caring for a baby in a spica cast requires specific instruction. Your doctor and healthcare team will teach you how to perform daily activities, maintain the cast, and identify any problems.
- 6 months to 2 years. Older babies are also treated with closed reduction and spica casting. In most cases, skin traction is used for a few weeks prior to repositioning the thighbone. Skin traction prepares the soft tissues around the hip for the change in bone positioning. It may be done at home or in the hospital.
Surgical Treatment
- 6 months to 2 years. If a closed reduction procedure is not successful in putting the thighbone is proper position, open surgery is necessary. In this procedure, an incision is made at the baby’s hip that allows the surgeon to clearly see the bones and soft tissues.
In some cases, the thighbone will be shortened in order to properly fit the bone into the socket. X-rays are taken during the operation to confirm that the bones are in position. Afterwards, the child is placed in a spica cast to maintain the proper hip position.
- Older than 2 years. In some children, the looseness worsens as the child grows and becomes more active. Open surgery is typically necessary to realign the hip. A spica cast is usually applied to maintain the hip in the socket.
Recovery
In many children with DDH, a body cast and/or brace is required to keep the hip bone in the joint during healing. The cast may be needed for 2 to 3 months. Your doctor may change the cast during this time period.
X-rays and other regular follow-up monitoring are needed after DDH treatment until the child’s growth is complete.
Complications
Children treated with spica casting may have a delay in walking. However, when the cast is removed, walking development proceeds normally.
The Pavlik harness and other positioning devices may cause skin irritation around the straps, and a difference in leg length may remain. Growth disturbances of the upper thighbone are rare, but may occur due to a disturbance in the blood supply to the growth area in the thighbone.
Even after proper treatment, a shallow hip socket may still persist, and surgery may be necessary in early childhood to restore the normal anatomy of the hip joint.
Outcomes
If diagnosed early and treated successfully, children are able to develop a normal hip joint and should have no limitation in function. Left untreated, DDH can lead to pain and osteoarthritis by early adulthood. It may produce a difference in leg length or a “duck-like” gait and decreased agility.
Even with appropriate treatment, hip deformity and osteoarthritis may develop later in life. This is especially true when treatment begins after the age of 2 years.
For More Information
If you found this article helpful, you may also be interested in Limb Length Discrepancy.
In order to assist doctors in the treatment of DDH, the American Academy of Orthopaedic Surgeons has done research to provide some useful guidelines. These are recommendations only and may not apply to each and every case. For more information: AAOS Clinical Practice Guideline: Detection and Nonoperative Management of Pediatric Developmental Dysplasia of the Hip in Infants Up to Six Months.

Reviewed by members of POSNA (Pediatric Orthopaedic Society of North America)
This article is also available in Spanish: Trombosis venosa profunda (Deep Vein Thrombosis).

Deep vein thrombosis, or DVT, occurs when a blood clot forms in one of the deep veins of the body. This can happen if a vein becomes damaged or if the blood flow within a vein slows down or stops. While there are a number of risk factors for developing a DVT, two of the most common are experiencing an injury to your lower body and having surgery that involves your hips or legs.
A DVT can have serious consequences. If a blood clot breaks free, it may travel through the bloodstream and block blood flow to the lungs. Although rare, this complication—called a pulmonary embolism—can be fatal. Even if a blood clot does not break free, it may cause permanent damage to the valves in the vein. This damage can lead to long-term problems in the leg such as pain, swelling, and leg sores.
In many cases, DVT occurs without noticeable symptoms and is very difficult to detect. For this reason, doctors focus on preventing the development of DVT using different types of therapies, depending upon a patient’s needs. Your doctor will take steps to prevent DVT if you have a major fracture or are having lower extremity surgery—including total hip or total knee replacement.
Description
Arteries are the blood vessels that carry oxygen-rich blood from the heart to all other parts of the body. Veins return the oxygen-depleted blood back to the heart. There are two types of veins in the body:
- Superficial veins lie just below the skin’s surface
- Deep veins are located deep within the muscles
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms within one of the deep veins. While DVT can occur in any deep vein, it most commonly occurs in the veins of the pelvis, calf, or thigh.
Cause
Several factors can affect blood flow in the deep veins and increase the risk for developing blood clots. These include:
- Increasing age
- Personal or family history of DVT or pulmonary embolism
- Having certain types of malignant cancers
- Having a vein disease, such as varicose veins
- Smoking
- Using birth control pills or hormone therapy
- Pregnancy
- Being overweight or obese
- Inheriting a blood-clotting disorder
A broken hip or leg, or having major surgery on your hip, knee or lower leg can affect normal blood flow and clotting. In these orthopaedic situations, three primary factors contribute to the formation of blood clots in veins: slow blood flow, hypercoagulation, and damage to the veins.
Blood that Flows Slowly through Veins (Stasis)
The walls of the veins are smooth. This helps blood flow freely and mix with naturally occurring agents (anticoagulants) in the blood that keep the blood cells from clotting. Blood that does not flow freely and does not mix with anticoagulants may be more likely to lead to blood clots. This is why it is important to watch for signs of DVT in people who are on bed rest, immobilized in a splint or cast, or not able to move for long periods of time.
Hypercoagulation
Blood thickens, or coagulates, around matter that does not belong in the veins. During surgery, matter such as tissue debris, collagen, or fat may be released into the blood system and can cause the blood to coagulate. In addition, during total hip replacement, reaming and preparing the bone to receive the prosthesis may cause the body to release chemical substances called antigens into the blood system. These antigens can also stimulate clot formation.
Damage to the Vein Walls
During surgery, the doctor must move, or retract, soft tissues such as ligaments, muscles, and tendons to reach the area being operated on. In some cases, this can release naturally occurring substances that promote blood clotting.
Complications
Pulmonary Embolism
A pulmonary embolism is a blood clot that breaks free and travels through the veins. This can happen right after the formation of the blood clot or it may happen days later. If the blood clot reaches the lungs, it can block the flow of blood to the lungs and heart.
A pulmonary embolism is a serious medical emergency and can lead to death.
Post-thrombotic Syndrome
Some people who have a DVT develop long-term symptoms in the calf, a condition called post-thrombotic syndrome. Post-thrombotic syndrome is caused when damage to the veins results in venous hypertension—or higher than normal blood pressure in the veins. This increased pressure can damage the valves that control blood flow through the veins. This allows blood to pool at the site—sometimes causing lasting impairment.
Patients with post-thrombotic syndrome may experience symptoms that can greatly impact the quality of life, including pain, swelling, skin changes, and leg sores.
Symptoms
Symptoms of DVT occur in the leg affected by the blood clot and include:
- Swelling
- Pain or tenderness
- Distended veins
- Red or discolored skin
- A firmness or thickening of the vein called a “cord”
Many patients, however, experience no symptoms at all.
In some cases, a pulmonary embolism may be the first sign of DVT. Symptoms of pulmonary embolism include:
- Shortness of breath
- Sudden onset of chest pain
- Coughing
- Spitting up or vomiting blood
Doctor Examination
If your doctor suspects DVT, he or she will order diagnostic tests.
Tests

Duplex ultrasound. This is the most common test for DVT. Ultrasound uses high-frequency sound waves that echo off the body—much like the technology used to check fetal well-being. This creates a picture of the blood vessels. Duplex ultrasound combines traditional ultrasound technology with Doppler technology, which generates a color image showing blood as it flows through the body.
Ultrasound is both noninvasive and painless. It can be repeated regularly because it does not require radiation. If you do not have a blood clot, duplex ultrasound may be helpful in revealing other causes for your symptoms.
Magnetic resonance imaging (MRI) scan. An MRI produces detailed, cross-sectional images of structures inside the body, including blood vessels and veins. The test is painless and noninvasive. Although used infrequently, some doctors may use an MRI to locate blood clots in the pelvis and thigh.
MRI allows both legs to be viewed at the same time. However, it cannot be used for patients with certain implanted devices, such as pacemakers.
Venography. In venography, the doctor injects a contrast solution (or dye) into a vein on the top of the foot. The solution mixes with the blood and flows throughout the veins. An x-ray of the affected leg will then show whether there are any blockages in the veins of the calf and thigh.
Venography is rarely used because it is invasive and requires radiation.
Treatment
Since DVT may occur after a major fracture or surgery, many patients are already hospitalized when the condition is diagnosed. The goals of treatment for DVT are to:
- Stop the blood clot from getting bigger
- Prevent the clot from breaking off and traveling to the lungs where it could lead to pulmonary embolism
- Reduce the chance of developing another clot
- Minimize the risk of developing other complications
Most often, treatment for DVT is nonsurgical.
Nonsurgical Treatment
Anticoagulants. Nonsurgical treatment usually consists of taking anticoagulants—blood thinning medications that will prevent further clotting and help dissolve existing clots. Anticoagulant medications are started immediately after the clot is diagnosed.
Anticoagulants can cause bleeding problems if the dosage is too high so their use must be monitored closely whether you are in the hospital or at home. Depending upon the medication you are taking, your doctor may order frequent blood tests to check how long it takes for your blood to clot. It is important to make sure that the medication level in your blood is high enough to prevent clots, but not too high to cause excessive bleeding.
The most common anticoagulants used to treat DVT are heparin, warfarin (Coumadin), and Xa inhibitors. In some cases, low molecular weight heparin (LMWH) may be used. LMWH is a type of anticoagulant derived from standard unfractionated heparin.
- Heparin. Treatment for DVT usually begins with heparin (or LMWH) therapy. Standard heparin is given intravenously (injection into a vein) while LMWH is given by subcutaneous injection under the skin. LMWH has a short half life and is eliminated from the body in 12 hours. Dosing is based on body weight. For most adults, each dose is the same—unlike for standard heparin, where doses are frequently changed based on clotting times.
Since LMWH does not require an intravenous line or dose monitoring it can be given on an outpatient basis. The injections are given either by a visiting nurse or performed by the patients themselves.
- Warfarin. Heparin (or LMWH) therapy is usually followed by 3 to 6 months of warfarin, which is taken orally. Warfarin takes at least 36 hours to start working, and from 4 to 5 days to reach its maximum effectiveness. For this reason, both heparin and warfarin are given at the start of treatment; the heparin protects the patient, keeping his or her blood anticoagulated until the warfarin “kicks in.”
- Xa inhibitors. These newer anticoagulants, taken orally, may work as well as warfarin in some patients. Because they do not require regular blood test monitoring or frequent adjustments in dosing, they are becoming more widely prescribed. There are risks and benefits to all types of anticoagulants. Your doctor will discuss which medication will work best for you.
Observation and serial ultrasound. Depending on your individual risk factors, your doctor may manage an isolated, below the knee or calf DVT with observation and monitoring through serial duplex ultrasound scans, rather than anticoagulant therapy. Your doctor will discuss which type of treatment is right for you.
Thrombolytics. In some cases, your doctor may recommend using thrombolytics. These clot-dissolving medications are injected via a catheter directly into the blood clot and are used only when there is an extremely high risk for pulmonary embolism.
Surgical Treatment
If anticoagulants do not stop your blood clot from increasing in size, or if you have a medical condition that does not allow you to take anticoagulation medications, your doctor may recommend surgery to insert a small device called a vena cava filter into the main vein leading to your heart. This filter is designed to capture most blood clots traveling through your blood stream before they reach your lungs and cause a pulmonary embolism.
Prevention
If you are having orthopaedic surgery, your risk for developing DVT is highest from 2 to 10 days after surgery and includes the time after you have been discharged from the hospital. You remain at risk for about 3 months.
The measures your doctor uses to help prevent DVT are called prophylaxis. He or she will use several preventive measures in combination. For example, if you are having total knee or total hip replacement, your doctor may prescribe early movement and exercise, compression stockings, and medications that thin the blood and reduce the body’s ability to form blood clots.
Early Movement and Physical Therapy
Most patients begin walking or doing other leg exercises as soon as possible after surgery. Performing simple leg lifts while lying in bed will help increase blood flow through the veins. In addition, a physical therapist will teach you specific exercises to restore joint range of motion, strengthen your lower body, and improve circulation in your deep veins. If pain after surgery makes it difficult for you to move, you may be given pain medication so that you can move more comfortably.
In some cases, your doctor may also use a knee support that slowly moves your knee while you are in bed. This device is called a continuous passive motion (CPM) machine. Some doctors believe the device decreases leg swelling by elevating your leg and improves blood circulation by moving the muscles of your leg.
Compression Devices

Graded elastic compression stockings are tight at the ankle and become looser as they go up the leg. The compression they provide may help circulation by preventing blood from pooling in the veins.
In addition, your doctor may recommend that you use an external pneumatic compression device after surgery. This device, which is worn like a boot, applies pulsing pressures to the calf. This pressure is similar to that which you experience while you are walking. Compression devices not only improve venous blood flow but also stimulate the body’s own ability to prevent blood clots.
Anticoagulants
Anticoagulants, or blood thinners, are used to stop blood clots from getting bigger and to prevent new blood clots from forming. If you are having joint replacement surgery, you will start anticoagulants the day after surgery and continue in the hospital and at home. The length of time that you take the medication will vary, depending on the type of surgery you have had, as well as other risk factors.
Additional Measures
If you have experienced a traumatic lower body injury, you may be treated with additional prophylactic measures. If you are unable to take anticoagulants, your doctor may implant a vena cava filter in the main vein leading to your heart. This is done to help prevent a potential DVT from reaching your heart and lungs and causing a pulmonary embolism.
The nerves in your body bring information to the brain about the environment (sensory nerves) and messages from the brain to activate muscles (motor nerves). To do this, nerves must pass over, under, around, and through your joints, bones, and muscles. Usually, there is enough room to permit easy passage.
Swelling, trauma, or pressure can narrow these openings and squeeze the nerve. When that happens, pain, paralysis, or other dysfunction may result.
A painful, burning sensation on the outer side of the thigh may mean that one of the large sensory nerves to your legs–the lateral femoral cutaneous nerve (LFCN)–is being compressed. This condition is known as meralgia paresthetica (me-ral’-gee-a par-es-thet’-i-ka).
- Pain on the outer side of the thigh, occasionally extending to the outer side of the knee
- A burning sensation, tingling, or numbness in the same area
- Occasionally, aching in the groin area or pain spreading across the buttocks
- Usually only on one side of the body
- Usually more sensitive to light touch than to firm pressure
During a physical examination, your physician will ask about recent surgeries, injury to the hip, or repetitive activities that could irritate the nerve. He or she will also check for any sensory differences between the affected leg and your other leg. To verify the site of the burning pain, the physician will put some pressure on the nerve to reproduce the sensation. You may need both an abdominal and a pelvic examination to exclude any problems in those areas.
X-rays will help identify any bone abnormalities that might be putting pressure on the nerve. If your physician suspects that a growth such as a tumor is the source of the pressure, he or she may ask for a magnetic resonance image or a computed tomography (CT) scan. In rare cases, a nerve conduction study may be advised.
Restrictive clothing and weight gain are two common reasons for pressure on a nerve. Your physician may ask if you wear a heavy tool belt at work or if you consistently wear a tight corset or girdle. He or she may recommend a weight loss program. Another reason may result from a seatbelt injury during a motor vehicle injury.
Treatments will vary, depending on the source of the pressure. It may take time for the burning pain to stop and, in some cases, numbness will persist despite treatment. The goal is to remove the cause of the compression. This may mean resting from an aggravating activity, losing weight, wearing loose clothing, or using a toolbox instead of wearing a tool belt. In more severe cases, your physician may give you an injection of a corticosteroid preparation to reduce inflammation. This generally relieves the symptoms for some time. In rare cases, surgery is needed to release the nerve.
If you found this article helpful, you may also be interested in Muscle Strains in the Thigh.
Before your joint replacement surgery, your doctor will discuss anesthesia with you. The selection of anesthesia is a major decision that could have a significant impact on your recovery. It deserves careful consideration and discussion with your surgeon and your anesthesiologist.
Several factors must be considered when selecting anesthesia, including:
- Your past experiences and preferences. Have you ever had anesthesia before? Did you have a reaction to the anesthesia? How do other members of your family react to anesthesia?
- Your current health and physical condition. Do you smoke? Are you overweight? Are you being treated for any condition other than your joint replacement?
- Your reactions to medications. Do you have any allergies? Have you ever experienced bad side effects from a drug? What medications, nutritional supplements, vitamins, or herbal remedies are you currently taking?
- The risks involved. Risks vary, depending on your health and selection of anesthesia, but may include breathing difficulties, allergic reactions and nerve injury. Your surgeon and anesthesiologist will discuss specific risks with you.
- Your healthcare team. The skills and preferences of your surgical and anesthesia team play an important role in the selection of anesthesia.
There are three broad categories of anesthesia: local, regional and general.
Local Anesthesia
Local anesthesia numbs only the specific area being treated. The area is numbed with an injection, spray or ointment that only lasts for a short period of time. Patients remain conscious during this type of anesthesia. This technique is reserved for minor procedures. For major surgery, such as hip or knee replacement, local anesthesia may be used to complement the main type of anesthesia that is used.
Regional Anesthesia
Regional anesthesia involves blocking the nerves to a specific area of the body, without affecting your brain or breathing. Because you remain conscious, you will be given sedatives to relax you and put you in a light sleep.
The three types of regional anesthesia used most frequently in joint replacement surgery are spinal blocks, epidural blocks and peripheral nerve blocks.
- Spinal Block. In a spinal block, the anesthesia is injected into the fluid surrounding the spinal cord in the lower part of your back. This produces a rapid numbing effect that wears off after several hours.
- Epidural Block. An epidural block uses a catheter inserted in your lower back to deliver local anesthetics over a variable period of time. The epidural block and the spinal block are administered in a very similar location; however, the epidural catheter is placed in a slightly different area around the spine as compared to a spinal block.
- Peripheral Nerve Block. A peripheral nerve block places local anesthetic directly around the major nerves in your thigh, such as the femoral nerve or the sciatic nerve. These blocks numb only the leg that is injected, and do not affect the other leg. One option for a peripheral block is to perform a one-time injection around the nerves in order to numb the leg just long enough for the surgery. Another option for this type of block is to keep a catheter in place, which can deliver continuous local anesthesia around the nerves for up to several days after surgery.
Advantages to regional anesthesia may include less blood loss, less nausea, less drowsiness, improved pain control after surgery, and reduced risk of serious medical complications, such as heart attack or stroke that — although rare — may occur with general anesthesia.
Side effects from regional anesthesia may include headaches, trouble urinating, allergic reactions, and rarely nerve injury.
General Anesthesia
General anesthesia is often used for major surgery, such as a joint replacement. General anesthesia may be selected based on patient, surgeon, or anesthesiologist preference, or if you are unable to receive regional or local anesthesia. Unlike regional and local anesthesia, general anesthesia affects your entire body. It acts on the brain and nervous system and renders you temporarily unconscious.
- Administration. With general anesthesia, the anesthesiologist administers medication through injection or inhalation. The anesthesiologist will also place a breathing tube down your throat and administer oxygen to assist your breathing.
- Risks. As with any anesthesia, there are risks, which may be increased if you already have heart disease, chronic lung conditions, or other serious medical problems.
General anesthesia affects both your heart and breathing rates, and there is a small risk of a serious medical complication, such as heart attack or stroke.
The tube inserted down your throat may give you a sore throat and hoarse voice for a few days.
Headache, nausea, and drowsiness are also common.
The goals of postoperative pain management are to minimize discomfort and allow you to move with less pain in order to participate in physical therapy after surgery. Postoperative pain relief may be achieved using a combination of oral medications or intravenous medications.
A common method of pain control is called “patient-controlled anesthesia” or “PCA.” With PCA, you will be able to control the flow of intravenous medication, within preset limits, as you feel the need for additional relief.
If an epidural or peripheral nerve block was used for your surgery, the epidural or peripheral catheter can be left in place and anesthesia can be continued in the postoperative period to help control pain. You may also have control over the amount of pain medication you receive in these catheters, within preset limits.
You will be closely monitored to avoid complications, such as excessive sedation or falls.
The proper use of pain relievers before, during and after your surgery is an extremely important aspect of your treatment. Proper use of pain medication can encourage healing and make your joint replacement a more satisfying experience. Take time to discuss the options with your doctor, and be sure to ask questions about things you do not understand.

Co-developed with the American Association of Hip and Knee Surgeons
Additional Resources on the Hip
Want more information? Try one of these websites. You will find information on musculoskeletal conditions relating to the hip, links to other websites, and information on other health conditions.
- American Association of Hip and Knee Surgeons
- Hip Society
- Medline Plus: Hip Injuries and Disorders
- National Institute for Arthritis and Musculoskeletal and Skin Disorders
- National Osteoporosis Foundation
This article is also available in Spanish: Actividades después de reemplazo de cadera (Activities After Hip Replacement).
After having a hip replacement, you may expect your lifestyle to be a lot like how it was before surgery—but without the pain. In many ways, you are right, but returning to your everyday activities will take time. Being an active participant in the healing process can help you get there sooner and ensure a more successful outcome.
Even though you will be able to resume most activities, you may have to change the way you do them. For example, you may have to learn new ways of bending down that keep your new hip safe. The suggestions you find here will help you enjoy your new hip while you safely resume your daily routines.
Your hospital stay will typically last from 1 to 4 days, depending on the speed of your recovery. Before you are discharged from the hospital, you will need to accomplish several goals, such as:
- Getting in and out of bed by yourself.
- Having acceptable pain control.
- Being able to eat, drink, and use the bathroom.
- Walking with an assistive device (a cane, walker, or crutches) on a level surface and being able to climb up and down two or three stairs.
- Being able to perform the prescribed home exercises.
- Understanding any hip precautions you may have been given to prevent injury and ensure proper healing.
If you are not yet able to accomplish these goals, it may be unsafe for you to go directly home after discharge. If this is the case, you may be temporarily transferred to a rehabilitation or skilled nursing center.
When you are discharged, your healthcare team will provide you with information to support your recovery at home. Although the complication rate after total hip replacement is low, when complications occur they can prolong or limit full recovery. Hospital staff will discuss possible complications, and review with you the warning signs of an infection or a blood clot.
Warning Signs of Infection
- Persistent fever (higher than 100 degrees)
- Shaking chills
- Increasing redness, tenderness or swelling of your wound
- Drainage from your wound
- Increasing pain with both activity and rest
Warning Signs of a Blood Clot
- Pain in your leg or calf unrelated to your incision
- Tenderness or redness above or below your knee
- Severe swelling of your thigh, calf, ankle or foot
In very rare cases, a blood clot may travel to your lungs and become life-threatening. Signs that a blood clot has traveled to your lungs include:
- Shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Notify your doctor immediately if you develop any of the above signs.
You will need some help at home for anywhere from several days to several weeks after discharge. Before your surgery, arrange for a friend, family member or caregiver to provide help at home.
Preparing Your Home
The following tips can help make your return home more comfortable, and can be addressed before your surgery:
- Rearrange furniture so you can maneuver with a cane, walker, or crutches. You may temporarily change rooms (make the living room your bedroom, for example) to minimize the use of stairs.
- Place items you use frequently (phone, remote control, glasses, pitcher and glass, reading material and medications, for example) within easy reach so you do not have to reach up or bend down.
- Remove any throw rugs or area rugs that could cause you to slip. Securely fasten electrical cords around the perimeter of the room.
- Get a good chair—one that is firm and has a higher-than-average seat. This type of chair is safer and more comfortable than a low, soft-cushioned chair.
- Install a shower chair, gripping bar, and raised toilet seat in the bathroom.
- Use assistive devices such as a long-handled shoehorn, a long-handled sponge, and a grabbing tool or reacher to avoid bending over too far.
![fig40 [Converted]](http://physicians.argusmso.com/dukeahn/files/2016/12/A00356F01.jpg)
Wound Care
During your recovery at home, follow these guidelines to take care of your wound and help prevent infection:
- Keep the wound area clean and dry. A dressing will be applied in the hospital and should be changed as often as necessary. Ask for instructions on how to change the dressing before you leave the hospital.
- Follow your doctor’s instructions on how long to wait before you shower or bathe.
- Notify your doctor immediately if the wound appears red or begins to drain. This could be a sign of infection.
Swelling
Expect mild to moderate swelling for 3 to 6 months after surgery. To reduce swelling, elevate your leg slightly and apply ice. Wearing compression stockings may also help reduce swelling. Notify your doctor if you experience new or severe swelling, since this may be the warning sign of a blood clot.
Medication
Take all medications as directed by your doctor. Home medications may include narcotic and non-narcotic pain pills, oral or injectable blood thinners, stool softeners, and anti-nausea medications.
Be sure to talk with your doctor about all your medications–even over-the-counter drugs, supplements, and vitamins. Your doctor will tell you which over-the-counter medicines are safe to take while using prescription pain medication.
It is especially important to prevent any bacterial infections from developing in your artificial joint. Your doctor may advise you to take antibiotics whenever there is the increased possibility of a bacterial infection, such as when you have dental work performed. Be sure to talk to your doctor before you have any dental work done and notify your dentist that you have had a hip replacement. You may also wish to carry a medical alert card so that, if an emergency arises, medical personnel will know that you have an artificial joint.
Diet
By the time you go home from the hospital, you should be eating a normal diet. Your doctor may recommend that you take iron and vitamin supplements. You also may be advised to avoid supplements that include vitamin K and foods rich in vitamin K if you are taking certain blood thinner medications, such as warfarin (Coumadin). Foods rich in vitamin K include broccoli, cauliflower, brussel sprouts, liver, green beans, garbanzo beans, lentils, soybeans, soybean oil, spinach, kale, lettuce, turnip greens, cabbage, and onions.
Continue to drink plenty of fluids, but try to limit coffee intake and avoid alcohol. You should continue to watch your weight to avoid putting more stress on the joint.
Once you get home, you should stay active. The key is to not do too much, too soon. While you can expect some good days and some bad days, you should notice a gradual improvement over time. Generally, the following guidelines will apply:
Weight Bearing
Follow your doctor’s specific instructions about the use of a cane, walker, or crutches and when you can put weight on the leg. Full weight bearing may be allowed immediately or may be delayed by several weeks depending on the type of hip replacement you have undergone and your doctor’s instructions.
Driving
In most cases, it is safe to resume driving when you are no longer taking narcotic pain medication, and when your strength and reflexes have returned to a more normal state. Your doctor will help you determine when it is safe to resume driving.
Sexual Activity
Please consult your doctor about how soon you can safely resume sexual activity. Depending on your condition, you may be able to resume sexual activity within several weeks after surgery.
Sleeping Positions
Depending on your surgery, your doctor may ask you to avoid certain sleeping positions or to sleep with a pillow between your legs for a length of time. Ask your doctor which sleeping positions are safest and most appropriate for you.
Return to Work
Depending on the type of activities you do on the job and the speed of your recovery, it may be several weeks before you are able to return to work. Your doctor will advise you when it is safe to resume your normal work activities.
Sports and Exercise
Continue to do the exercises prescribed by your physical therapist for at least 2 months after surgery. In some cases, your doctor may recommend riding a stationary bicycle to help maintain muscle tone and keep your hip flexible.
As soon as your doctor gives you the go-ahead, you can return to many of the sports activities you enjoyed before your hip replacement:
- Walk as much as you would like, but remember that walking is no substitute for the exercises prescribed by your doctor and physical therapist.
- Swimming is an excellent low-impact activity after a total hip replacement; you can begin as soon as the sutures have been removed and the wound is healed.
- In general, lower impact fitness activities such as golfing, bicycling, and light tennis, put less stress on your hip joint and are preferable over high-impact activities such as jogging, racquetball and skiing.
Air Travel
Pressure changes and immobility may cause your hip joint to swell, especially if it is just healing. Ask your doctor before you travel on an airplane. When going through security, be aware that the sensitivity of metal detectors varies and your artificial joint may cause an alarm. Tell the screener about your artificial joint before going through the metal detector. You may also wish to carry a medical alert card to show the airport screener.
Dos and don’ts (precautions) vary depending on your doctor’s surgical technique. Your doctor and physical therapist will provide you with a list of dos and don’ts to remember with your new hip. These precautions will help to prevent the new joint from dislocating and ensure proper healing. Here are some of the most common precautions:
The Don’ts
- Don’t cross your legs at the knees for at least 6 to 8 weeks.
- Don’t bring your knee up higher than your hip.
- Don’t lean forward while sitting or as you sit down.
- Don’t try to pick up something on the floor while you are sitting.
- Don’t turn your feet excessively inward or outward when you bend down.
- Don’t reach down to pull up blankets when lying in bed.
- Don’t bend at the waist beyond 90 degrees.
The Dos
- Do keep the leg facing forward.
- Do keep the affected leg in front as you sit or stand.
- Do use a high kitchen or barstool in the kitchen.
- Do kneel on the knee on the operated leg (the bad side).
- Do use ice to reduce pain and swelling, but remember that ice will diminish sensation. Don’t apply ice directly to the skin; use an ice pack or wrap it in a damp towel.
- Do apply heat before exercising to assist with range of motion. Use a heating pad or hot, damp towel for 15 to 20 minutes.
- Do cut back on your exercises if your muscles begin to ache, but don’t stop doing them!
Here are some exercises that your doctor may recommend:
Low Impact Aerobic Exercise – Swimming and riding a stationary bike are great low impact exercises that help build strength. Stop any exercise that causes increasing pain.
Short-Arc Knee Extensions – Roll up several towels in a roll 6-8 inches thick. Lay in bed with the towels under one knee. Bend the other knee. Keeping your knee on the towels, lift your foot to straighten the knee. Hold for a few seconds and lower the foot.
Ankle Pumps – While lying in bed, point your toes downward and then bring your toes back up towards your head, tightening your calf.
Heel Slides – Slide your heel along the bed pulling your foot towards you as your knee bends.
Straight Leg Raise – Start by tightening your quadriceps, the muscles in the front of your thigh. Then with toes toward the ceiling, lift your leg 6-12 inches from the bed.
Quadriceps Sets – Lie on your back, legs straight. Tighten the muscle in the front of your thigh as you press the back of your knee toward the bed. Hold for a few seconds, then relax the leg.
Standing Knee Bends – Stand while holding onto a steady surface, such as a table. Bend your knee as far as it will go comfortably. Hold for a few seconds and lower the leg.
Increasing upper body strength is also important because of the need to use a walker or crutches after surgery.
Bicep Curls – In a sitting position, keep you elbow close to your body and your wrist straight. Bend you arm, moving your hand up to your shoulder, then lower slowly.
Triceps Extensions – Sit, leaning forward from the waist. Bend your elbow so that your forearm is parallel to the floor. Then straighten your elbow as you extend your arm behind you.
Seated Press Ups – Sit in a sturdy chair with armrests. With palms on the armrests, press down to lift yourself from the chair. Hold for 3-5 seconds. Bend your elbows slowly to ease back down.
Talk to your doctor before starting any exercise program and remember to call your doctor if you experience increased pain or swelling after exercise.
Ceramic Materials Offer the Potential for a Longer-Lasting Hip Replacement

Conventional hip replacement systems use an insert made of plastic and a head made of metal. Over time, these components may wear as the parts move back and forth with normal joint use. Eventually, this may lead to the joint wearing out, and an additional surgery or “revision” is needed to replace the worn-out joint.
As total hip replacement becomes more common in younger and more active patients, and as patient life expectancies continue to increase, the orthopaedic industry has been challenged to extend the life span of total hip replacement components.
The clinical use of ceramic as a bearing surface dates back to the early 1970s. In 1995, an improved alumina ceramic was developed that had increased purity and strength over the first generation materials. The type of ceramic used in total hip replacement today is aluminum oxide, also known as alumina.
The extreme hardness of this type of ceramic offers greater scratch resistance than the conventional implants used in conventional hip replacements.1 Ceramic-on-ceramic surfaces have demonstrated significantly lower wear versus conventional plastic-on-metal hip systems in the laboratory.2 Therefore, it is anticipated that these improved wear characteristics may extend the life of the implant.
The best type of replacement for you depends on your medical condition, activity level, and age. Talk to your orthopaedic specialist to find out if a ceramic-on-ceramic hip replacement is right for you.
What is a Hip Replacement?
Hip replacement involves the removal of arthritic bone ends and damaged cartilage and replaces them with prosthetic implants that replicate the hip joint. Hip replacement can help relieve pain and get you back to enjoying normal, everyday activities.
What Are the Reasons for Total Hip Replacement?
Total hip replacement is often reserved for patients who:
- Have a painful, disabling joint disease of the hip resulting from a severe form of arthritis.
- Are not likely to achieve satisfactory results from less invasive procedures, such as arthrodesis (artificial stiffening or fixation of the joint).
- Have bone stock that is of poor quality or inadequate for other reconstructive techniques.
How is a Total Hip Replacement Performed?
In a total hip replacement operation, the surgeon replaces the worn surfaces of the hip joint with an artificial hip joint. The worn head of the femur (thighbone) is replaced with a metal or ceramic ball mounted on a stem; the stem is placed firmly into the canal of the thighbone at its upper end. The acetabulum (hip socket) is prepared and implanted with a metal cup and plastic or ceramic insert. The ball and insert glide together to replicate the hip joint.
Who Should Have a Hip Replacement?
Hip replacement surgery may be considered when arthritis limits your everyday activities such as walking and bending, when pain continues while resting, or stiffness in your hip limits your ability to move or lift your leg. Hip replacement may be recommended only after careful diagnosis of your joint problem. It may be time to consider surgery if you have little pain relief from anti-inflammatory drugs, or if other treatments, such as physical therapy, do not relieve hip pain.
How Long is the Hospital Stay?
After hip replacement surgery, you will probably spend no more than three to five days in the hospital. Most hip replacement patients begin standing and walking with the help of a walker and a physical therapist the day after surgery. However, everyone is different, and you should discuss what you can expect with your doctor.
How Long is Recuperation?
Recovery varies with each person. It is essential that you follow your orthopaedic surgeon’s instructions regarding home care during the first few weeks after surgery; especially concerning the exercise program you are prescribed. You should be able to resume most normal light activities of daily living within three to six weeks following surgery. Some discomfort during activity and at night is common for several weeks. Complete recovery can take from about three to six months.
While most people will gradually increase their activities and return to doing things like playing golf, doubles tennis, shuffleboard, or bowling, you will be advised to avoid more active sports, such as jogging, singles tennis, and other high-impact activities.
Are There Complications?
As with any surgery, there is a risk of complications after hip replacement surgery. However, they are relatively rare. Blood clots are the most common complication after surgery. Your orthopaedic surgeon may prescribe one or more measures to prevent a clot from forming in your leg veins. These measures may include a special support hose, inflatable leg coverings, and blood thinners.
What is the Success Rate?
Hip replacement is one of the most important surgical advances of this century. This surgery helps more than 300,000 Americans each year to relieve their pain, and get back to enjoying normal, everyday activities.1
How Long Does a Hip Replacement Last?
The conventional arrangement of a metal ball into a special plastic (polyethylene) cup has been shown to have positive results over the years. How long it will last depends not only on age, but also a patient’s activity level. Newer hip replacement materials using more durable alumina ceramic and titanium have made major advances in hip replacement technology. Demand and activity levels are generally considered when the surgeon works with you to decide which type of hip replacement materials are best for you.
Your joints are involved in almost every activity you do. Simple movements such as walking, bending, and turning require the use of your hip and knee joints. Normally, all parts of these joints work together and the joint moves easily without pain. But when the joint becomes diseased or injured, the resulting pain can severely limit your ability to move and work. Osteoarthritis, one of the most common forms of degenerative joint disease, affects an estimated 43 million people in the United States.1 Whether you are considering a total joint replacement, or are just beginning to explore available treatments, this website is for you. It will help you understand the causes of joint pain and treatment options. Most importantly, it will give you hope that you may be able to return to your favorite activities.
Once you’re through reading this website, be sure to ask your doctor any questions you may have. Gaining as much knowledge as possible will help you choose the best course of treatment to relieve your joint pain — and get you back into the swing of things.
Hip Anatomy and Function
How a Healthy Hip Works
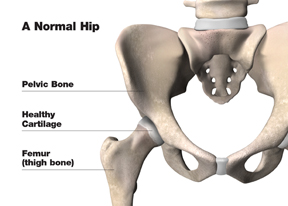
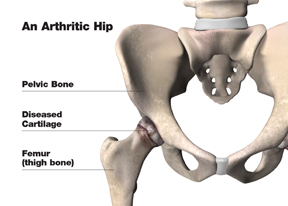
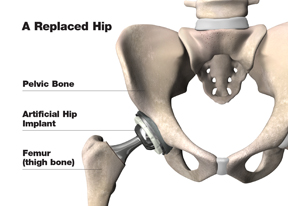
The hip is one of the main weight-bearing joints in your body. It consists of two main parts:
- A ball (femoral head) at the top of your thighbone (femur)
- A rounded socket (acetabulum) in your pelvis
Ligaments, which are bands of tissue, connect the ball to the socket and help keep the ball and socket steady. A smooth, tough material called articular cartilage, which cushions the bones and lets them move easily, covers the surfaces of the ball and socket.
All the rest of the surfaces of the hip joint are covered by a thin, smooth tissue liner called synovial membrane, which makes a small amount of fluid that acts as a lubricant so that the bones in the hip joint will not rub against each other.
What causes hip pain?
Pain in your hip can be debilitating, making it difficult for you to walk, climb stairs, or even pick up an object from the floor. It can limit your freedom of movement and ability to function independently.
While hip pain can be caused by deformity or by direct injury, like trauma or a sports injury, the most common cause of hip pain is osteoarthritis (OA) also known as degenerative joint disease (DJD). Depending on factors like age, weight, joint function, and activity, people with arthritis find their hip’s cartilage lining wears away over time. At that point, your bones begin to rub against each other, resulting in friction, swelling, pain, stiffness, and instability.
Experiencing joint pain day after day without relief can lead to “staying off” the joint — which often weakens the muscles around it so it becomes even more difficult to move.
Your Treatment Options for Hip Pain
You don’t have to live with severe joint pain and the functional limitations it causes. If you have not experienced adequate results with medication and other conservative treatments, total joint replacement may provide the pain relief you long for, in addition to allowing you to return to the lifestyle and activities you enjoy. Your orthopaedic specialist can tell you whether you might benefit from joint replacement and explain the reasons why it may, or may not, be right for you.
Of course, even if your orthopaedic specialist determines that joint replacement is a good medical option for you, it is still up to you to make the final decision. The ultimate goal is for you to be as comfortable as possible, and that always means making the best decision for you based on your own individual needs.
About Total Hip Replacement
Hip replacement surgery involves replacing the femur (head of the thighbone) and the acetabulum (hip socket). Typically, the artificial ball with its stem is made of a strong metal or ceramic, and the artificial socket is made of polyethylene (a durable, wear-resistant plastic) or metal backed with a plastic liner. The artificial joint may be cemented in position or held securely in the bone without cement.
Joint Pain – Understanding the Causes and Treatment Options
Don’t Let Joint Pain Slow You Down
Your joints are involved in almost every activity you do. Simple movements such as walking, bending, and turning require the use of your hip and knee joints. Normally, all parts of these joints work together and the joint moves easily and without pain. But when the joint becomes diseased or injured, the resulting pain can severely limit your ability to move and work.
Whether you are considering a total joint replacement, or are just beginning to explore available treatments, this website is for you. It will help you understand the causes of joint pain and treatment options. Most importantly, it will give you hope that you will be able to do more of the things you enjoy — with far less pain.
Once you’re through reading this website, be sure to ask your doctor any questions you may have. Gaining as much knowledge as possible will help you choose the best course of treatment to help relieve your joint pain — and get you back into the swing of things.
Physical Therapy
Physical therapy can be helpful in the management of Osteoarthritis (OA) and Rheumatoid Arthritis (RA). For example, a physical therapist may recommend:
- Isometric (“pushing”) exercises to help build muscle strength without subjecting inflamed joints to excessive wear
- Isotonic (“pulling”) exercises to further increase muscle strength and help preserve function
- Daily walking, using a cane or other assistive device as needed
Joint Fluid Supplements
For patients whose joint pain does not improve with medication or physical therapy, “joint grease” injections may provide temporary relief. The joint is injected with a joint fluid supplement that acts as a lubricant for the damaged joint. Joint injection schedules and duration of relief vary according to the treatment chosen and the individual patient. However, these injections do not cure the diseased joint and joint replacement may be needed as the joint worsens with time.
Nutritional Supplements
Glucosamine and Chondroitin
Your doctor has provided this information to answer some of the questions you may have about nutritional supplements that may be linked to improved joint health. The possible beneficial effects of glucosamine and chondroitin, two popular supplements for patients with joint pain, have been making news in recent years. This information is intended to help you better understand who might benefit from the supplements and why.
What are glucosamine and chondroitin?
Glucosamine and chondroitin are actually two different molecules found in healthy joint cartilage. The medical theory behind taking these supplements is that they would help the body repair cartilage that has been broken down by osteoarthritis (the most common “wear-and-tear” form of arthritis). Some popular glucosamine supplements are derived from shellfish; chondroitin supplements are often derived from shark or cattle. Both can also be made synthetically. The supplements are sold and packaged much in the same way vitamins are. Like vitamins, they are not subject to review or approval by the U.S. Food and Drug Administration.
Do glucosamine and chondroitin help reduce arthritis pain?
Although the U.S. Food and Drug Administration has tentatively concluded that no studies to date have linked glucosamine and chondroitin to a reduced risk of developing osteoarthritis1, a large study administered by the National Institutes of Health has shown that glucosamine and chondroitin, when taken together, significantly reduce pain in patients with moderate-to-severe osteoarthritis of the knee.2 In fact, the study showed that people taking the supplements experienced the same amount of pain relief as people who took non-steroidal anti-inflammatory medications (NSAIDs)3 – long the go-to medication for people with arthritis pain. What sounds even better, treatment with glucosamine and chondroitin supplements has not been associated with any side effects. NSAIDs, on the other hand, have been associated with gastrointestinal side effects, including bleeding.3
Make a Plan with Your Doctor
Don’t assume that your doctor will not take your interest in nutritional supplements seriously. Many doctors understand how some supplements can complement your current arthritis treatment plan.4 Your doctor can also help you determine if a particular supplement is right for you given your overall health. Your doctor can also help monitor the effectiveness of your supplement regimen.
A Word of Caution
Because vitamins and other nutritional supplements are not monitored by any federal agency to assure purity or dosage, you’ll want to do your homework before you purchase or consume anything. Look for a familiar, reputable brand name. If you have questions about the product, write to the manufacturer for more information. Ask your doctor about his or her experience with the supplement. And, most importantly, if you experience any adverse reactions, stop taking the supplement and call your doctor right away.
For more information on glucosamine and chondroitin, talk with your doctor or visit the National Institutes of Health website at www.nih.gov.
Treatment Options
Following the orthopaedic evaluation, the orthopaedic specialist will review and discuss the results with you. Based on his or her diagnosis, your treatment options may include:
Non Surgical Options
Diet & Exercise
- Average American is 20–40 lbs. overweight.
- Average person takes 5000–7000 steps/day.
- Reduces stress on weight-bearing joints (extra pressure on some joints may aggravate your arthritis).
- A balanced diet helps manage weight and stay healthy.
ROM Exercises
- Maintains normal joint movement.
- Increases flexibility.
- Relieves stiffness.
Strengthening Exercises
- Increasing muscle strength helps support and protect joints affected by arthritis.
- Exercise is an important part of arthritis treatment that is most effective when done properly and routinely.
Aerobic Exercise
- Improve cardiovascular fitness.
- Helps control weight.
- May help reduce inflammation in joints.
Rest & Joint Care
- Short-term bed rest helps reduce both joint inflammation and pain, and is especially useful when multiple joints are affected and fatigue is a major problem.
- Individual joint rest is most helpful when arthritis involves one or only a few joints.
- Heat Therapy (increases blood flow, tolerance for pain, flexibility).
- Cold Therapy — cold packs, ice massage, OTC sprays and ointments (reduces pain by numbing the nerves around the joint).
Osteoporosis FAQs
What is Osteoporosis?
Osteoporosis is a skeletal disease characterized by low bone mass that results in a reduction in the strength of the skeleton.
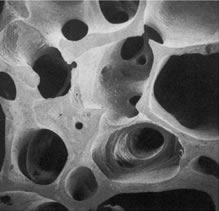
Normal Bone |
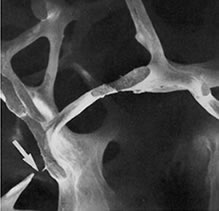
Osteoporotic Bone |
The Scope of the Problem
- Osteoporosis affects as many as 44 million Americans
- 80% of those affected are women
- One in two women and one in four men over age 50 will have an osteoporosis-related fracture in her/his remaining lifetime
- While osteoporosis is often thought of as an older person’s disease, it can strike at any age
Consequences of Osteoporosis
- Increased risk of fracture of the hip, spine, and wrist
- Morbidity and mortality from fracture
– Over 300,000 hip fractures/year
– A 50-year-old white woman has a 15% lifetime probability of suffering a hip fracture - Healthcare costs
– 2002: $18 billion
Fractures of the Hip and Spine
Osteoporosis
Osteoporosis is a disease in which bones grow more fragile and porous over time, making them more likely to break. Often known as the “silent disease,” osteoporosis is painless and many people don’t even know they have it until they suffer a broken bone after a minor injury, or begin to lose height. Sometimes the only symptom is a dull pain that is felt, in the hips, lower back, neck and wrists.
Generally, our bones reach a peak bone density at 25 to 30 years of age. Shortly afterward, we begin to lose bone density. Osteoporosis is diagnosed when a significant amount of density within our bones has been depleted.
Certain people are at higher risk of developing osteoporosis than others. Risk factors include: *
- Being female
- Family history of osteoporosis
- Thin or small frame
- Postmenopausal
- Vitamin and nutritional deficiencies
- Diet low in calcium
- Inactive lifestyle
- Caucasian or Asian ethnicity
- Certain medications like corticosteroids or anticonvulsants
- Low estrogen levels in women
- Low testosterone levels in men
- Excessive use of alcohol
- Cigarette smoking
* http://www.nof.org/osteoporosis/diseasefacts.htm – February, 2006
Testing for Osteoporosis
Treatment for osteoporosis involves preventing further bone weakening, building bone density, preventing bone fractures, and managing any pain you have. But first, you must be diagnosed. A simple, painless screening called a bone mineral density (BMD) test is used to
- Identify osteoporosis before a fracture occurs
- Predict your chances of fracturing in the future
- Determine your rate of bone loss
- Monitor the effects of any treatment
In a BMD test, you simply lie on a padded table beneath a scanning device. The technician uses a small amount of radiation, or sound waves, to collect information about your bone mass. The results are then compared to normal values. If you are identified as having signs of osteoporosis, certain treatments can help slow bone loss and reduce your risk of fracture. Identifying osteoporosis early is important. Plus, most private insurance carriers and Medicare now cover BMD testing for certain individuals. BMD testing is safe, painless, and noninvasive; it is recommended that all women over age 65 be tested.
Osteoporosis Treatment
Treatment for osteoporosis involves preventing further bone weakening, building bone density, preventing bone fractures, and managing the pain associated with the disease. It is recommended that people of all ages engage in regular weight-bearing exercises, such as walking, riding a stationary bike, or jogging. Supplementing your diet with 1,200 to 1,500 mg of calcium and 600 to 800 IU of vitamin D daily can also help to keep your bones strong. In some cases, your doctor may discuss estrogen replacement or other medications that strengthen the bones by increasing the density and preventing further bone loss.
If you suspect that you have signs or symptoms of osteoporosis or have risk factors for osteoporosis, please see your doctor for further evaluation and treatment.
Understanding Osteonecrosis
Your doctor has provided this information to answer some of the questions you may have about osteonecrosis and how it may affect you. It will also help you better understand what to expect when osteonecrosis has an impact on your joints and requires medical treatment.
What is osteonecrosis (ON)?
Osteonecrosis is a disease that results from a loss of blood supply to the bone. Without adequate blood flow, sections of bone eventually die, weaken and collapse. Because this is most often seen at the ends of bones, your joints may be greatly affected. This is especially true of the hip joint, as osteonecrosis most commonly appears at the end of the femur (the long bone that extends from the knee to the hip joint). Medical experience has shown that wherever osteonecrosis causes bone to degrade in a joint, arthritis develops.1, 2
You may hear osteonecrosis referred to as avascular necrosis, asceptic necrosis and ischemic necrosis. The word osteonecrosis literally means “dead bone”.
Who does ON affect?
Each year between 10,000 and 20,000 men and women develop osteonecrosis.3 Although ON can affect anyone at any age, most people who develop ON are between 30 and 50 years old.1 Orthopaedic surgeons have found that in as many as ten percent of all people requiring hip replacement, osteonecrosis has led to their joint damage.
Even though medical science has learned a lot about osteonecrosis and its potential causes, research into contributing genetic risk factors is ongoing. To date, we know that you may be at an increased risk for developing ON if you’ve dislocated or fractured a hip, suffer with alcoholism, use corticosteroids, or have any number of glandular diseases, including rheumatoid arthritis, Gaucher’s disease, chronic pancreatitis, Crohn’s disease or lupus.3
What are the symptoms of ON?
Patients with early stage osteonecrosis may not have any symptoms. Later symptoms include pain, diminished range of motion and the development of osteoarthritis. Osteonecrosis progresses differently in each person affected by it, however the time between feeling the first symptoms of joint pain and losing joint function is usually anywhere from a few months to over a year.1
In order to diagnose you properly, your doctor will consider your symptoms and your medical history, examine your joint(s) and order one or more diagnostic tests. Your doctor may order X-rays, a CT scan, bone scan, a biopsy or an MRI to get a clear view of your condition.
How is ON treated?
Your doctor may recommend different treatment options depending on the severity of your ON and its impact on your joint(s) and your body as a whole. Your doctor may be especially interested in the condition of your femur and whether the head of the bone is still intact.
Manage the pain and preserve your joint.
Your doctor’s priorities will include alleviating your pain, improving your function, preventing further joint damage and saving as much of your natural bone as possible. To accomplish this, you may be treated with very specific medications in order to slow the progression of the disease, joint deformity and loss of function.1 Your doctor may prescribe any one of these medications, or a combination of several: non-steroidal anti-inflammatory medications (NSAIDs), blood thinners (to increase blood flow to the affected bone) or cholesterol-lowering medications (often called statins), especially if corticosteroid use has elevated your cholesterol level.
Get the right support.
Your doctor may recommend that you reduce weight bearing on the affected joint. That may mean that you’ll be asked to use a crutch or limit your activities to permit your joint to heal while you’re under treatment. Your doctor may also recommend some range-of-motion exercises, or even prescribe a course of physical therapy so a trained therapist can guide you through specific movements. Some studies have shown that electrical stimulation (a painless, non-invasive therapy) may promote healthy new bone growth.1
Understand your surgical options.
If you are still experiencing pain and joint damage that’s affecting your quality of life even after all other conservative measures have been taken, your doctor may suggest surgery to help relieve your pain and restore your mobility. Your doctor will determine the proper surgical treatment based on the severity of your condition. Today, a full range of surgical solutions exist that enable your doctor to customize surgical procedures to your particular needs and anatomy, whether you need core decompression, osteotomy (re-shaping the bone), bone grafting (which may help your body create healthy new blood vessels and bone cells) or arthroplasty (replacing the affected joint).
For people diagnosed with osteonecrosis, treatment and medical management of the disease may continue throughout their lifetime. Be sure to talk with your doctor about the best treatment option for you.
Understanding Rheumatoid Arthritis
What is rheumatoid arthritis (RA)?
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s natural immune response wreaks havoc on the lining of the joints (called the synovial membrane), causing chronic inflammation and pain.1The inflammation may eventually damage the joint’s cartilage and bone, weaken the soft tissue around the joint (cartilage, ligaments and tendons) and prevent the joint from working properly.1
Who does RA affect?
More than two million people in the United States have been diagnosed with RA.2 RA can affect anyone at any age, but women appear especially at risk. In fact, women develop RA more than twice as often as men.3 Although the medical community does not know what causes RA, today’s best research has identified a genetic marker, found in white blood cells, that may help doctors determine if a particular person is at an increased risk.2, 3
What are the symptoms of RA?
RA is a chronic, persistent disease that seems to take its own course over an affected person’s lifetime. It may progress slowly, sometimes produce “flare ups” of symptoms, and then at times go into “remission” during which the symptoms may greatly diminish or disappear. Unfortunately, RA never seems to go away completely.
Doctors sometimes talk about the three stages of RA. Those stages are identified by specific symptoms. In the first stage, RA causes pain, warmth, redness and swelling in affected joints. In the second stage, it causes thickening of the joint lining. In the third, permanent joint damage begins to occur as bone and cartilage are attacked by the enzymes released by the inflamed cells in the affected joint’s once-healthy cushioning fluid (called synovial fluid).1, 4
In addition to joint pain, swelling and stiffness, the symptoms of RA commonly include fatigue, weakness, flu-like symptoms accompanied by a low-grade fever, loss of appetite, depression, chronic dry eye or dry mouth and, in people with more advanced RA, bumps (called rheumatoid nodules) under the skin.1, 5
Without question, left untreated, RA can greatly reduce your quality of life. You may have already begun to decrease your activity level just to avoid the pain caused by a joint affected by RA. It’s not uncommon for the joint damage caused by RA to lead to a loss of movement, an inability to work, and even the need for surgery to repair the damage.4
In order to diagnose you properly, your doctor will consider your symptoms and your medical history, examine your joint(s) and order one or more diagnostic tests. Your doctor may order blood work, X-rays, a CT scan or an MRI to get a clear view of your condition.
How is RA treated?
Your primary doctor will refer you to a rheumatologist, a doctor who specializes in inflammatory diseases like RA. Your rheumatologist may recommend different treatment options depending on the severity of your RA and its impact on your joint(s) and your body as a whole. And while there is no cure, RA can be controlled through the use of new drugs, exercise, joint protection techniques and self-management techniques.
Manage the pain and preserve your joint.
Today, most doctors understand the value of treating RA more aggressively with very specific medications in order to slow the progression of the disease, joint deformity and loss of function.1 Your doctor may prescribe any one of these medications, or a combination of several: non-steroidal anti-inflammatory medications (NSAIDs), analgesics, steroids, disease modifying anti-rheumatic drugs (DMARDs) or biologic response modifiers that work on the immune system.
Look at the big picture.
Your doctor may recommend that you modify your diet, take certain nutritional supplements, exercise and get adequate sleep. Your doctor may also encourage you to learn about how managing your stress and learning some relaxation techniques may help improve your quality of life and help you to handle your RA symptoms with greater ease.6
Understand your surgical options.
If you are still experiencing arthritis pain and joint damage that’s affecting your quality of life even after all other conservative measures have been taken, your doctor may suggest surgery to help relieve your pain and restore your mobility. Your doctor will determine the proper surgical treatment based on the severity of your arthritis. Today, a full range of surgical solutions exist that enable your doctor to customize surgical procedures to your particular needs and anatomy, whether you need arthroscopic debridement (removing inflamed and/or irritating debris from the joint), arthrodesis (fusing the joint for greater support) or arthroplasty (replacing the arthritic joint).
Be sure to talk with your doctor about the best treatment option for you.
Understanding Osteoarthritis
What is osteoarthritis (OA)?
Osteoarthritis (OA) is the most common form of arthritis in the world.1 You may have heard OA referred to as “wear and tear” arthritis. When OA begins to affect one of your joints, a series of reactions take place that actually begin to degrade your once-healthy bone and the “soft tissue” around the joint – tendons and cartilage. Once the cartilage that normally cushions and protects the bones of the joint breaks down, the bones of your joint eventually rub directly against each other. Your body reacts to this by creating bone spurs and the joint capsule itself may thicken and weaken. Inflammation eventually sets in.
Doctors talk about two kinds of OA. Primary OA often refers to “everyday wear”; Secondary OA is considered the result of a malaligned joint, being overweight, injury or overuse.1, 2
Who does OA affect?
Twenty-one million people are affected by OA in the United States alone.3 Although OA can affect anyone at any age, it has been linked to the aging process. More than 50% of everyone over 65 has OA symptoms in one or both knees. By 75, virtually everyone suffers with OA in one or more joints. In fact, OA of the knee and hips continues to be the most common cause of arthritis-related disability for Americans. The Arthritis Foundation cites that men and women may develop OA at different times in life. Most people develop symptoms after 45, but, as a group, men under 55 and women over 55 develop OA more frequently.
What are the symptoms of OA?
Although some people who have osteoarthritis say they feel no pain, most people who have OA experience pain, feel joint stiffness (especially in the morning), show signs of swelling and tenderness in one or more joints and may even hear a crunching sound in their joints. For some people, OA can become completely debilitating.3
In order to diagnose you properly, your doctor will consider your symptoms and your medical history, examine your joint(s) and order one or more diagnostic tests. Your doctor may order blood work, X-rays, a CT scan or an MRI to get a clear view of the alignment of your painful joint and its condition.
How is OA treated?
Your doctor may recommend different treatment options depending on the severity of your osteoarthritis and its impact on your joint(s).
Manage the pain.
Your doctor may prescribe or recommend the use of anti-inflammatory medications (like aspirin or ibuprofen) and cold packs that may help to reduce inflammation as well as the pain associated with arthritis. Sometimes a local injection of cortisone helps to further reduce inflammation.
Look at the big picture.
Your doctor may recommend that you lose weight, take certain nutritional supplements and exercise. In some cases, a physical therapist may help provide pain relief and the return of some lost mobility through guided exercise and other techniques.
Get the right support.
Orthotic devices sometimes help. Custom-made shoes and shoe inserts provide support for those with OA in the foot or ankle. Your doctor may recommend a brace or a cane to help take some of the pressure off your affected joint while you walk if OA is affecting your knee or hip.
Understand your surgical options.
If you are still experiencing arthritis pain and joint damage that’s affecting your quality of life even after all other conservative measures have been taken, your doctor may suggest surgery to help relieve your pain and restore your mobility. Your doctor will determine the proper surgical treatment based on the severity of your arthritis and its location. Today, a full range of surgical solutions exist that enable your doctor to customize surgical procedures to your particular needs and anatomy, whether you need arthroscopic debridement (removing inflamed and/or irritating debris from the joint), arthrodesis (fusing the joint for greater support) or arthroplasty (replacing the arthritic joint).
Be sure to talk with your doctor about the best treatment option for you.
Arthritis
Osteoarthritis (OA)
Osteoarthritis is sometimes called degenerative arthritis because it is a “wearing out” condition involving the breakdown of cartilage in the joints. Joint cartilage is a gel-like protective tissue found at joint surfaces that provides support and lubrication during movement. When cartilage wears away, the bones rub against each other, causing pain and stiffness. OA usually occurs in people over age 50, and often in people with a family history of osteoarthritis.
Rheumatoid Arthritis (RA)
This disease produces chemical changes that cause the synovial membrane (the membrane that surrounds the joint) to become thickened and inflamed. In turn, too much synovial fluid (the fluid that lubricates the joints) is produced. The result of this chronic inflammation is cartilage loss, pain, and stiffness. RA affects women about three times more often than men,* and may affect other organs of the body, including the skin and heart.**
*www.mothernature.com
**www.jointpainny.com
Post-Traumatic Arthritis
This condition may develop after an injury to the joint in which the bone and cartilage do not heal properly. The joint is no longer smooth, and these irregularities lead to more wear on the joint.
Paget’s Disease
This is a bone disease that often affects the hip, in which bone formation is accelerated. The density and shape of the bone changes, which in turn causes bone pain and inflammation of the joints.
Avascular Necrosis
This disease can result when a bone is deprived of its normal blood supply, which may happen after organ transplantation or long-term cortisone treatment. Without proper nutrition from the blood, the bone’s structure weakens and may collapse and damage the cartilage.
Osteoarthritis – Definition
Osteoarthritis, sometimes referred to as degenerative joint disease, is a type of arthritis that affects the cartilage around joints. Joint cartilage is a gel-like protective tissue found at joint surfaces that provides support and lubrication during movement. When the surface layer of this tissue breaks down, the bones rub together during joint movement, causing pain, swelling, and restricted movement. Although it can occur in any joint, osteoarthritis most often involves the hands, knees, hips, and spine.
It is thought that a number of factors cause this condition, including the natural aging process, joint injury, and repetitive stress from certain jobs or sports activities. Diabetes, gout, and some genetic conditions may also put you at risk.
Osteoarthritis Treatment
The treatment for osteoarthritis concentrates on preventing further joint damage. Lifestyle changes such as weight loss, joint strengthening exercises, and assistant devices (orthoses) are recommended. Physical therapy may also help restore joint movement.
Your doctor may initially suggest acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) to minimize pain. In later stages of the disease, several surgical options may need to be discussed. Arthroscopy, for example, entails using a camera to examine the joint and repair the cartilage at the joint surface. Arthrodesis involves the surgical fusion of the bony ends of the joint. Replacement with an artificial joint to maintain function is yet another surgical option.
If you suspect that you have signs or symptoms of osteoarthritis or have risk factors for osteoarthritis, please see your doctor to discuss further evaluation and treatment.
When a joint is healthy, all of the parts work together and the joint moves easily and without pain. However, diseases or injury can disturb the normal functioning of your joints resulting in:
- Pain
- Muscle weakness
- Limited movement
Arthritis is one of the most common causes of joint disorders. More than 42 million people in the United States are diagnosed with arthritis.* The most common types of arthritis are:
- Osteoarthritis
- Rheumatoid Arthritis
- Post-Traumatic Arthritis
- Paget’s Disease
- Avascular Necrosis
Other causes of joint pain are deformity or direct injury to the joint. And sometimes, regardless of the cause of your pain, it can be made worse when you avoid using your joint altogether. That’s because with less use, the muscles around your joint weaken, which can make it even more difficult and painful to move.
