Transient osteoporosis of the hip is an uncommon condition that causes temporary bone loss in the upper portion of the thighbone (femur).
People with transient osteoporosis of the hip will experience a sudden onset of pain that intensifies with walking or other weight-bearing activities. In many cases, the pain increases over time and may become disabling.
Painful symptoms gradually subside and usually end within 6 to 12 months. Bone strength in the hip also returns to normal in the majority of people.
Despite the name, transient osteoporosis of the hip is very different from the more common age-related osteoporosis. Age-related osteoporosis is a painless, progressive condition that leads to a weakening of the bones throughout the body. Unlike transient osteoporosis, it can put people at greater long-term risk for fractures in different areas of the body.
For more information about age-related osteoporosis: Osteoporosis
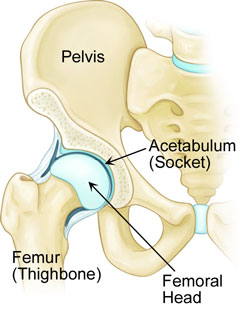
The hip is one of the body’s largest joints. It is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
In transient osteoporosis of the hip, the femoral head loses density and strength.
Description
Transient osteoporosis of the hip is an uncommon condition that most often occurs in young or middle-aged men (between ages 30 and 60), and in women in the late stages of pregnancy (the last 3 months) or in the early post-partum period.
Transient osteoporosis most often occurs in the hip joint, but can also affect other joints in the leg, such as the knee, ankle and foot.
During the time that the bone is weakened, it is at greater risk for breaking.
Cause
Currently, there is no clear explanation for what causes this condition. Researchers are studying this disease and several theories have been proposed, although none are proven.
Some of the causes that have been suggested include:
- Obstruction of some of the small blood vessels that surround the hip
- Hormonal changes
- Abnormal mechanical stresses on the bone
Symptoms
- Sudden onset of pain, typically in the front of the thigh, the groin, the side of the hip, or the buttocks.
- Pain that intensifies with weight bearing and may lessen with rest.
- No previous accident or injury to the joint that would trigger pain.
- Slightly limited motion: gentle hip motion is usually painless, but pain may intensify with extreme motions of the hip.
- Pain that gradually increases over a period of weeks or months and may be so intense that it is disabling.
- A noticeable limp as the patient tries to protect the joint and ease the pain.
Doctor Examination
Because transient osteoporosis of the hip is not a common condition, doctors often diagnose it by ruling out other, more frequent sources of hip pain. Arthritis, osteonecrosis, stress fracture, muscle injury, and tumor are all conditions that your doctor may consider during your evaluation.
Medical History and Physical Examination

Your doctor will talk to you about your symptoms and when they first began. He or she may ask you whether you can remember any injury to the joint.
During the physical examination, your doctor will have you move your leg in different directions to assess your range of motion and try to replicate the pain. Most patients with transient osteoporosis of the hip have more pain when they move the hip themselves (active range of motion) as opposed to when the doctor moves the hip for them (passive range of motion). In addition, pain is often felt only with extremes of hip movements, and it usually worsens with any weight bearing. This discrepancy (severe pain with weight bearing, but minimal pain with passive range of motion) is one of the clues to the diagnosis of transient osteoporosis.
Tests
-
- X-rays. In the early course of the disease (the first 6 weeks), x-ray images may show a subtle decrease in the bone density of the femoral head, but this may be hard to see. Several months later, x-rays may show a dramatic loss of bone density with a near complete disappearance of the femoral head. This temporary loss of bone density is why the disease is termed “transient osteoporosis of the hip.”

-
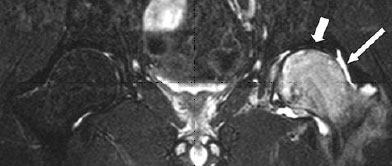
- Other imaging scans. Because x-rays may not show bone loss until the condition is well-advanced, your doctor may order other types of imaging tests to identify the cause of your symptoms. Computed tomography (CT) scans and
magnetic resonance imaging (MRI) scans can provide more detailed images. MRI scans provide clear images of the soft tissues surrounding the hip. A nuclear medicine bone scan can more clearly show changes in bone caused by infection or
injury. (A nuclear medicine bone scan should not be confused with a Dual Energy X-ray Absortiometry (DEXA) scan. A DEXA scan is a study that tests for generalized bone density, and while it is the gold-standard in testing for age-related
osteoporosis, it is not effective in diagnosising transient osteoporosis of the hip.)
- Other imaging scans. Because x-rays may not show bone loss until the condition is well-advanced, your doctor may order other types of imaging tests to identify the cause of your symptoms. Computed tomography (CT) scans and
If you are pregnant, your doctor may decide to delay imaging studies until the last stages of your pregnancy, or even until after the delivery. Generally, MRI is safe to obtain in pregnancy, although you should discuss this with your orthopaedic surgeon,your primary doctor, and your obstetrician if you are considering this test.
- Laboratory tests. Currently there is no blood test that helps to diagnose this disorder. However, blood tests are often very helpful in ruling out other causes of hip pain, such as metabolic (nutritional) disorders, endocrine(hormonal) disorders, and metastatic disease (cancer).
Bone Marrow Edema
One of the most common signs of transient osteoporosis of the hip is bone marrow edema. Bone marrow is a spongy substance that produces blood cells and is located in the hollow of long bones. In bone marrow edema, the bone marrow is inflamed and full of fluid.
An MRI scan of a hip affected by transient osteoporosis will usually reveal bone marrow edema. Because of this, MRI is one of the most useful studies to help diagnose the condition.
Treatment
Because transient osteoporosis resolves on its own, treatment focuses on minimizing symptoms and preventing any damage to the bones while they are weakened by the disorder.
- Non-steroidal anti-inflammatory medication (NSAIDs). Drugs like ibuprofen and naproxen may relieve pain and inflammation.
- Weight bearing restrictions. Your doctor may advise you to temporarily limit or completely eliminate weight-bearing activities. Using crutches, a cane, a walker, or other walking aid, will help relieve the stress of weight bearing on the hip, and may prevent a fracture through the temporarily weakened bone.
- Physical therapy. To help maintain strength and flexibility in the muscles supporting your hip, your doctor may also recommend a series of exercises that you can do as the pain subsides. Water exercises may be helpful not only because they ease movement, but also because they relieve weight bearing.
- Nutrition. Proper nutrition, including Vitamin D and calcium, may help promote the healing process and rebuilding of bone.
Outcomes
With proper diagnosis and treatment, most patients with transient osteoporosis of the hip can expect complete resolution of symptoms within 6 to 12 months. Bone strength in the hip also will return to normal in the majority of cases.
In a small percentage of patients, transient osteoporosis recurs later in life. It can return to the same hip or even in the opposite hip. Whether the condition will recur is difficult to predict.
