Deep vein thrombosis, or DVT, occurs when a blood clot forms in one of the deep veins of the body. This can happen if a vein becomes damaged or if the blood flow within a vein slows down or stops. While there are a number of risk factors for developing a DVT, two of the most common are experiencing an injury to your lower body and having surgery that involves your hips or legs.
A DVT can have serious consequences. If a blood clot breaks free, it may travel through the bloodstream and block blood flow to the lungs. Although rare, this complication—called a pulmonary embolism—can be fatal. Even if a blood clot does notbreak free, it may cause permanent damage to the valves in the vein. This damage can lead to long-term problems in the leg such as pain, swelling, and leg sores.
In many cases, DVT occurs without noticeable symptoms and is very difficult to detect. For this reason, doctors focus on preventing the development of DVT using different types of therapies, depending upon a patient’s needs.
Your doctor will take steps to prevent DVT if you have a major fracture or are having lower extremity surgery—including total hip or total knee replacement.
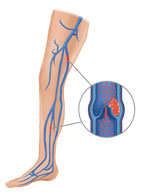
Blood clots may form in one of the deep veins of the body.
Description
Arteries are the blood vessels that carry oxygen-rich blood from the heart to all other parts of the body. Veins return the oxygen-depleted blood back to the heart. There are two types of veins in the body:
- Superficial veins lie just below the skin’s surface
- Deep veins are located deep within the muscles
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms within one of the deep veins. While DVT can occur in any deep vein, it most commonly occurs in the veins of the pelvis, calf, or thigh.
<iframe width=”520″ height=”360″ class=”youtube-embed” src=”http://www.youtube.com/embed/xM44LqJDNXA?wmode=opaque&rel=0″ frameborder=”0″ wmode=”opaque” allowfullscreen=””></iframe>
Cause
Several factors can affect blood flow in the deep veins and increase the risk for developing blood clots. These include:
- Increasing age
- Personal or family history of DVT or pulmonary embolism
- Having certain types of malignant cancers
- Having a vein disease, such as varicose veins
- Smoking
- Using birth control pills or hormone therapy
- Pregnancy
- Being overweight or obese
- Inheriting a blood-clotting disorder
A broken hip or leg, or having major surgery on your hip, knee or lower leg can affect normal blood flow and clotting. In these orthopaedic situations, three primary factors contribute to the formation of blood clots in veins: slow blood flow, hypercoagulation,and damage to the veins.
Blood that Flows Slowly through Veins (Stasis)
The walls of the veins are smooth. This helps blood flow freely and mix with naturally occurring agents (anticoagulants) in the blood that keep the blood cells from clotting. Blood that does not flow freely and does not mix with anticoagulants may be more likely to lead to blood clots. This is why it is important to watch for signs of DVT in people who are on bed rest, immobilized in a splint or cast, or not able to move for long periods of time.
Hypercoagulation
Blood thickens, or coagulates, around matter that does not belong in the veins. During surgery, matter such as tissue debris, collagen, or fat may be released into the blood system and can cause the blood to coagulate. In addition, during total hip replacement, reaming and preparing the bone to receive the prosthesis may cause the body to release chemical substances called antigens into the blood system. These antigens can also stimulate clot formation.
Damage to the Vein Walls
During surgery, the doctor must move, or retract, soft tissues such as ligaments, muscles, and tendons to reach the area being operated on. In some cases, this can release naturally occurring substances that promote blood clotting.
Complications
Pulmonary Embolism
A pulmonary embolism is a blood clot that breaks free and travels through the veins. This can happen right after the formation of the blood clot or it may happen days later. If the blood clot reaches the lungs, it can block the flow of blood to the lungs
and heart.
A pulmonary embolism is a serious medical emergency and can lead to death.
<iframe width=”520″ height=”360″ class=”youtube-embed” src=”http://www.youtube.com/embed/teDMDE3CUfM?wmode=opaque&rel=0″ frameborder=”0″ wmode=”opaque” allowfullscreen=””></iframe>
Post-thrombotic Syndrome
Some people who have a DVT develop long-term symptoms in the calf, a condition called post-thrombotic syndrome. Post-thrombotic syndrome is caused when damage to the veins results in venous hypertension—or higher than normal blood pressure in the veins. This increased pressure can damage the valves that control blood flow through the veins. This allows blood to pool at the site—sometimes causing lasting impairment.
Patients with post-thrombotic syndrome may experience symptoms that can greatly impact the quality of life, including pain, swelling, skin changes, and leg sores.
Symptoms
Symptoms of DVT occur in the leg affected by the blood clot and include:
- Swelling
- Pain or tenderness
- Distended veins
- Red or discolored skin
- A firmness or thickening of the vein called a “cord”
Many patients, however, experience no symptoms at all.
In some cases, a pulmonary embolism may be the first sign of DVT. Symptoms of pulmonary embolism include:
- Shortness of breath
- Sudden onset of chest pain
- Coughing
- Spitting up or vomiting blood
Doctor Examination
If your doctor suspects DVT, he or she will order diagnostic tests.
Tests
combines traditional ultrasound technology with Doppler technology, which generates a color image showing blood as it flows through the body.Ultrasound is both noninvasive and painless. It can be repeated regularly because it does not require radiation.
If you do not have a blood clot, duplex ultrasound may be helpful in revealing other causes for your symptoms.
 (Left) In an ultrasound, the technician places a noninvasive probe called a “transducer” over the patient’s leg. (Right) The transducer sends images to the ultrasound machine and screen.Magnetic resonance imaging (MRI) scan. An MRI produces detailed, cross-sectional images of structures inside the body, including blood vessels and veins. The test is painless and noninvasive. Although used infrequently, some doctors
(Left) In an ultrasound, the technician places a noninvasive probe called a “transducer” over the patient’s leg. (Right) The transducer sends images to the ultrasound machine and screen.Magnetic resonance imaging (MRI) scan. An MRI produces detailed, cross-sectional images of structures inside the body, including blood vessels and veins. The test is painless and noninvasive. Although used infrequently, some doctorsmay use an MRI to locate blood clots in the pelvis and thigh.MRI allows both legs to be viewed at the same time. However, it cannot be used for patients with certain implanted devices, such as pacemakers.Venography. In venography, the doctor injects a contrast solution (or dye) into a vein on the top of the foot. The solution mixes with the blood and flows throughout the veins. An x-ray of the affected leg will then show whether there are any blockages in the veins of the calf and thigh.Venography is rarely used because it is invasive and requires radiation.
Treatment
Since DVT may occur after a major fracture or surgery, many patients are already hospitalized when the condition is diagnosed. The goals of treatment for DVT are to:
- Stop the blood clot from getting bigger
- Prevent the clot from breaking off and traveling to the lungs where it could lead to pulmonary embolism
- Reduce the chance of developing another clot
- Minimize the risk of developing other complications
Most often, treatment for DVT is nonsurgical.
Nonsurgical Treatment
Anticoagulants. Nonsurgical treatment usually consists of taking anticoagulants—blood thinning medications that will prevent further clotting and help dissolve existing clots. Anticoagulant medications are started immediately
after the clot is diagnosed.
Anticoagulants can cause bleeding problems if the dosage is too high so their use must be monitored closely whether you are in the hospital or at home. Depending upon the medication you are taking, your doctor may order frequent blood tests to
check how long it takes for your blood to clot. It is important to make sure that the medication level in your blood is high enough to prevent clots, but not too high to cause excessive bleeding.
The most common anticoagulants used to treat DVT are heparin, warfarin (Coumadin), and Xa inhibitors. In some cases, low molecular weight heparin (LMWH) may be used. LMWH is a type of anticoagulant derived from standard unfractionated heparin.
-
- Heparin. Treatment for DVT usually begins with heparin (or LMWH) therapy. Standard heparin is given intravenously (injection into a vein) while LMWH is given by subcutaneous injection under the skin. LMWH has a short half
life and is eliminated from the body in 12 hours. Dosing is based on body weight. For most adults, each dose is the same—unlike for standard heparin, where doses are frequently changed based on clotting times.
- Heparin. Treatment for DVT usually begins with heparin (or LMWH) therapy. Standard heparin is given intravenously (injection into a vein) while LMWH is given by subcutaneous injection under the skin. LMWH has a short half
Since LMWH does not require an intravenous line or dose monitoring it can be given on an outpatient basis. The injections are given either by a visiting nurse or performed by the patients themselves.
- Warfarin. Heparin (or LMWH) therapy is usually followed by 3 to 6 months of warfarin, which is taken orally. Warfarin takes at least 36 hours to start working, and from 4 to 5 days to reach its maximum effectiveness. For this
reason, both heparin and warfarin are given at the start of treatment; the heparin protects the patient, keeping his or her blood anticoagulated until the warfarin “kicks in.” - Xa inhibitors. These newer anticoagulants, taken orally, may work as well as warfarin in some patients. Because they do not require regular blood test monitoring or frequent adjustments in dosing, they are becoming more widely
prescribed. There are risks and benefits to all types of anticoagulants. Your doctor will discuss which medication will work best for you.
Observation and serial ultrasound. Depending on your individual risk factors, your doctor may manage an isolated, below the knee or calf DVT with observation and monitoring through serial duplex ultrasound scans, rather than anticoagulant
therapy. Your doctor will discuss which type of treatment is right for you.
Thrombolytics. In some cases, your doctor may recommend using thrombolytics. These clot-dissolving medications are injected via a catheter directly into the blood clot and are used only when there is an extremely high risk for
pulmonary embolism.
Surgical Treatment
If anticoagulants do not stop your blood clot from increasing in size, or if you have a medical condition that does not allow you to take anticoagulation medications, your doctor may recommend surgery to insert a small device called a vena cava filter into the main vein leading to your heart. This filter is designed to capture most blood clots traveling through your blood stream before they reach your lungs and cause a pulmonary embolism.
Prevention
If you are having orthopaedic surgery, your risk for developing DVT is highest from 2 to 10 days after surgery and includes the time after you have been discharged from the hospital. You remain at risk for about 3 months.
The measures your doctor uses to help prevent DVT are called prophylaxis. He or she will use several preventive measures in combination. For example, if you are having total knee or total hip replacement, your doctor may prescribe early movement
and exercise, compression stockings, and medications that thin the blood and reduce the body’s ability to form blood clots.
Early Movement and Physical Therapy
Most patients begin walking or doing other leg exercises as soon as possible after surgery. Performing simple leg lifts while lying in bed will help increase blood flow through the veins. In addition, a physical therapist will teach you specific
exercises to restore joint range of motion, strengthen your lower body, and improve circulation in your deep veins. If pain after surgery makes it difficult for you to move, you may be given pain medication so that you can move more comfortably.
In some cases, your doctor may also use a knee support that slowly moves your knee while you are in bed. This device is called a continuous passive motion (CPM) machine. Some doctors believe the device decreases leg swelling by elevating your
leg and improves blood circulation by moving the muscles of your leg.
Compression Devices
Graded elastic compression stockings are tight at the ankle and become looser as they go up the leg. The compression they provide may help circulation by preventing blood from pooling in the veins.
In addition, your doctor may recommend that you use an external pneumatic compression device after surgery. This device, which is worn like a boot, applies pulsing pressures to the calf. This pressure is similar to that which you experience while
you are walking. Compression devices not only improve venous blood flow but also stimulate the body’s own ability to prevent blood clots.

Anticoagulants
Anticoagulants, or blood thinners, are used to stop blood clots from getting bigger and to prevent new blood clots from forming. If you are having joint replacement surgery, you will start anticoagulants the day after surgery and continue
in the hospital and at home. The length of time that you take the medication will vary, depending on the type of surgery you have had, as well as other risk factors.
Additional Measures
If you have experienced a traumatic lower body injury, you may be treated with additional prophylactic measures. If you are unable to take anticoagulants, your doctor may implant a vena cava filter in the main vein leading to your heart.
This is done to help prevent a potential DVT from reaching your heart and lungs and causing a pulmonary embolism.
