Arthritis involves inflammation of one or more of your joints. Pain and stiffness are common symptoms of arthritis, and when these occur in your wrist, simple daily activities can become more difficult.
There are many types of arthritis, and most of these can affect the wrist. Although the severity of symptoms related to arthritis can vary, most arthritis-related diseases are chronic. This means that they are long-lasting—even permanent—and can eventually cause serious joint damage.
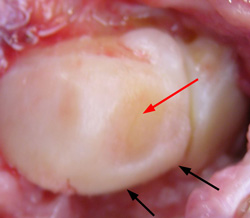
Your wrist is a complex joint—it is actually made up of multiple small joints. When healthy, the bones glide easily over each other during movement, protected by smooth cartilage that coats the joint surfaces. Arthritis damages this cartilage. As the disease progresses, there is a gradual loss of cartilage. Without a smooth joint surface, the bones rub against each other, leading to joint damage that cannot be repaired.
Although there is no cure for arthritis today, there are many treatment options available to help relieve your symptoms. Some options may also slow the progression of joint damage. With proper treatment, many people are able to manage their symptoms and stay active.
Anatomy
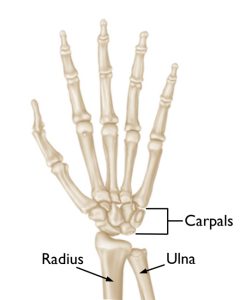
The wrist is a complex joint that connects the hand to the forearm. It is formed by the two bones of the forearm—the radius and the ulna—and eight small carpal bones. The carpal bones are arranged in two rows at the base of the hand. There are four bones in each row.
The joint surface of each bone is covered with articular cartilage—a slippery substance that protects and cushions the bones as you move your hand and wrist.
Description
Although there are many types of arthritis, the three that most commonly affect the wrist are:
- Osteoarthritis
- Rheumatoid arthritis
- Posttraumatic arthritis
Osteoarthritis
Osteoarthritis can develop due to normal “wear-and-tear” in the wrist, particularly in people who have a family history of arthritis. It is a common problem for many people after they reach middle age, though it may occur in younger people, too.
In osteoarthritis, the smooth, slippery articular cartilage that covers the ends of the bones gradually wears away over time. Because the cartilage surface has little to no blood supply, it has little ability to heal or regenerate when it becomes injured or worn down.
As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone and lead to pain and stiffness in the joint.

Osteoarthritis in the wrist can also develop from Kienböck’s disease. In Kienböck’s disease, the blood supply to one of the carpal bones—the lunate—is disrupted, causing the bone to die and slowly collapse. Over time, this collapse can lead to changes and arthritis in the joints around the lunate.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body. The condition often starts in smaller joints, such as those found in the hand and wrist. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the body’s immune system attacks its own tissues. In rheumatoid arthritis, the defenses that normally protect the body from infection instead damage normal tissue (such as cartilage and ligaments) and can soften bone.
Rheumatoid arthritis often affects the joint between the two bones of the forearm, the radius and ulna. The deformity in the ulna can cause wearing and possible rupture of the tendons that straighten your fingers. This can cause more deformity and loss of function in your hand.
The exact cause of rheumatoid arthritis is not known—there are no clear genetic or environmental factors. Although it is not an inherited disease, researchers believe that some people have genes that could make them more likely to have rheumatoid disease.

Posttraumatic Arthritis
Posttraumatic arthritis can develop after an injury, such as a broken wrist bone or a torn ligament. This trauma can cause a direct injury to the cartilage or a delayed wearing of the cartilage due to a change in the way the bones move together—such as after a ligament tear.
Posttraumatic arthritis can develop over many years from the initial injury. Despite proper treatment, an injured joint is more likely to become arthritic over time.
Symptoms
Not all patients with arthritis will experience symptoms. When they do occur, the severity varies greatly from patient to patient. For some patients, the symptoms are not constant—but may come and go depending on their level of activity and other factors.
Symptoms of arthritis may include:
- Pain
- Swelling
- Reduced range of motion or stiffness
- Weakness in the joint
Doctor Examination
Physical Examination
Your doctor will talk with you about your overall health and medical history and ask you to describe your symptoms. He or she will perform a careful examination of your hand and wrist, looking for:

- Reduced range of motion
- Any areas of pain or tenderness
- Joint instability
- Swelling or other changes in appearance
During the examination, your doctor may also evaluate:
- Finger and thumb mobility—To determine how well your tendons and joints are functioning
- Nerve function—To determine if you have another condition that may be affecting your wrist, such as carpal tunnel syndrome (nerve compression)
Tests
X-rays. X-rays provide detailed images of dense structures, such as bone. X-rays of your wrist will help your doctor learn more about the exact location and severity of your arthritis. They can also help your doctor distinguish between various types of arthritis.
Blood tests. Your doctor may recommend blood tests to determine which type of arthritis you have. With rheumatoid and other types of inflammatory arthritis, blood tests are important for an accurate diagnosis. Osteoarthritis is not associated with blood abnormalities.
Treatment
There is no cure for arthritis, but there are a number of treatments that may help reduce the frequency of your symptoms and relieve the pain and loss of function it can cause.
Nonsurgical Treatment
In general, initial treatment for arthritis is nonsurgical in nature and designed to help minimize your symptoms.
Nonsurgical treatment options may include:
- Activity modification. Limiting or stopping the activities that make your pain worse is the first step in relieving symptoms.
- Immobilization. Wearing a wrist splint for a short time will help support the joint and ease the stress placed on it by frequent use and activities.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, naproxen, and ibuprofen can help reduce both pain and swelling. Topical NSAIDs can be applied directly to the skin in the area of the joint.
- Exercise. Specific exercises will help improve range of motion and function in your wrist. Your doctor or a physical therapist can help develop an exercise program that meets your specific needs.
- Steroid injection. Cortisone is a powerful anti-inflammatory agent that can be injected into an arthritic joint. Although an injection of cortisone can provide relief and reduce inflammation, the effects may be temporary.
- Other therapies. This may include using “contrast soaks” of warm and cold water to help reduce swelling.
If your symptoms of rheumatoid arthritis are not adequately controlled by the above therapies, your doctor may prescribe additional medications. These medications—called disease-modifying anti-rheumatic drugs (DMARDs)—are designed to stop the immune system from attacking the joints.
Like all medications, DMARDs have both risks and benefits. Your use of DMARDs will be directed by a rheumatologist.
Surgical Treatment
If nonsurgical treatment does not relieve your pain and your quality of life has been significantly affected by arthritis, your doctor may recommend surgery.
The goal of surgery is to relieve pain while preserving or improving hand function. Typically, this is done by minimizing or eliminating bone-on-bone contact. There are a number of procedures for arthritis of the wrist. Your doctor will talk with you about which procedure will work best in your case.
Proximal row carpectomy. In this procedure, your doctor removes three carpal bones in the row of bones that is closest to the forearm. The procedure is designed to reduce your pain while maintaining some wrist motion.

Fusion. If motion is the source of your pain, your doctor may recommend fusion. Fusion is essentially a “welding” process. The basic idea is to fuse together the bones so that they heal into a single, solid bone. The theory behind fusion is that, if the painful bones do not move, they should not hurt.
During the procedure, your doctor removes the damaged cartilage and then uses pins, plates, or screws to hold the joint in a permanent position. Over time, the bones fuse or grow together— similar to the way the fractured ends of a bone heal together.
In some cases, your doctor can perform a partial fusion in which just some of the carpal bones are fused together. This addresses the damaged joint surfaces, but leaves the healthy joints intact to preserve some wrist motion.

If your arthritis is extensive, however, a complete wrist fusion may be necessary. In this procedure, all of the carpal bones are fused together, along with the radius (one of the bones in the forearm). Although all wrist motion is eliminated in a complete fusion, forearm rotation and finger/thumb motion are generally preserved.

Total wrist replacement (arthroplasty). In total wrist replacement, your doctor removes the damaged cartilage and bone in your wrist and then positions new metal or plastic joint surfaces to restore the function of the joint. Replacing the wrist joint relieves the pain of arthritis while allowing more wrist movement than fusion.

Living with Arthritis
It can be discouraging to learn that you have arthritis, but there are some things you can do to help lessen the impact the condition has on your life. These include:
- Talk to your doctor. If your symptoms worsen or you are having a hard time coping, ask your doctor to review your treatment plan and determine if changes are needed.
- Change your activities. If certain activities aggravate your arthritis, cut down or eliminate these activities to help minimize your symptoms.
- Try alternative therapies. Some alternative therapies appear to help arthritis pain. Always talk to you doctor before trying any alternative treatments as they may interfere with your overall treatment plan.
If you found this article helpful, you may also be interested in Carpal Tunnel Syndrome.
