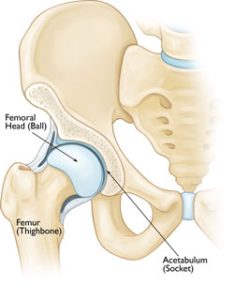
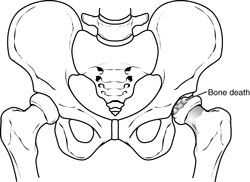
Perthes disease is a rare childhood condition that affects the hip. It occurs when the blood supply to the rounded head of the femur (thighbone) is temporarily disrupted. Without an adequate blood supply, the bone cells die, a process called avascular necrosis.
Although the term “disease” is still used, Perthes is really a complex process of stages that can last several years. As the condition progresses, the weakened bone of the head of the femur (the “ball” of the “ball-and-socket” joint of the hip) gradually begins to break apart. Over time, the blood supply to the head of the femur returns and the bone begins to grow back.
Treatment for Perthes focuses on helping the bone grow back into a more rounded shape that still fits into the socket of the hip joint. This will help the hip joint move normally and prevent hip problems in adulthood.
The long-term prognosis for children with Perthes is good in most cases. After 18 months to 2 years of treatment, most children return to daily activities without major limitations.
Description
Perthes disease — also known as Legg-Calve-Perthes, named for the three individual doctors who first described the condition — typically occurs in children who are between 4 and 10 years old. It is five times more common in boys than in girls, however,it is more likely to cause extensive damage to the bone in girls. In 10% to 15% of all cases, both hips are affected.
There are four stages in Perthes disease:
- Initial / necrosis. In this stage of the disease, the blood supply to the femoral head is disrupted and bone cells die. The area becomes intensely inflamed and irritated and your child may begin to show signs of the disease, such as a limp or different way of walking. This initial stage may last for several months.
- Fragmentation. Over a period of 1 to 2 years, the body removes the dead bone and quickly replaces it with an initial, softer bone (“woven bone”). It is during this phase that the bone is in a weaker state and the head of the femur is more likely to break apart and collapse.
- Reossification. New, stronger bone develops and begins to take shape in the head of the femur. The reossification stage is often the longest stage of the disease and can last a few years.
- Healed. In this stage, the bone regrowth is complete and the femoral head has reached its final shape. How close the shape is to round will depend on several factors, including the extent of damage that took place during the fragmentation phase, as well as the child’s age at the onset of disease, which affects the potential for bone regrowth.
Cause
The cause of Perthes disease is not known. Some recent studies indicate that there may be a genetic link to the development of Perthes, but more research needs to be conducted.
Symptoms
One of the earliest signs of Perthes is a change in the way your child walks and runs. This is often most apparent during sports activities. Your child may limp, have limited motion, or develop a peculiar running style. Other common symptoms include:
- Pain in the hip or groin, or in other parts of the leg, such as the thigh or knee (called “referred pain.”).
- Pain that worsens with activity and is relieved with rest.
- Painful muscle spasms that may be caused by irritation around the hip.
Depending upon your child’s activity level, symptoms may come and go over a period of weeks or even months before a doctor visit is considered.
Doctor Examination
After discussing your child’s symptoms and medical history, your doctor will conduct a thorough physical examination.

-
- Physical examination tests. Your doctor will assess your child’s range of motion in the hip. Perthes typically limits the ability to move the leg away from the body (abduction), and twist the leg toward the inside of the body (internal rotation).
- X-rays. These scans create pictures of dense structures like bone, and are required to confirm a diagnosis of Perthes. X-rays will show the condition of the bone in the femoral head and help your doctor determine the stage of the disease.
A child with Perthes can expect to have several x-rays taken over the course of treatment, which may be 2 years or longer. As the condition progresses, x-rays often look worse before gradual improvement is seen.
Treatment
The goal of treatment is to relieve painful symptoms, protect the shape of the femoral head, and restore normal hip movement. If left untreated, the femoral head can deform and not fit well within the acetabulum, which can lead to further hip problems in adulthood, such as early onset of arthritis.
There are many treatment options for Perthes disease. Your doctor will consider several factors when developing a treatment plan for your child, including:
- Your child’s age. Younger children (age 6 and below) have a greater potential for developing new, healthy bone.
- The degree of damage to the femoral head. If more than 50% of the femoral head has been affected by necrosis, the potential for regrowth without deformity is lower.
- The stage of disease at the time your child is diagnosed. How far along your child is in the disease process affects which treatment options your doctor will recommend.
Nonsurgical Treatment
Observation. For very young children (those 2 to 6 years old) who show few changes in the femoral head on their initial x-rays, the recommended treatment is usually simple observation. Your doctor will regularly monitor your child using x-rays to make sure the regrowth of the femoral head is on track as the disease runs its course.
Anti-inflammatory medications. Painful symptoms are caused by inflammation of the hip joint. Anti-inflammatory medicines, such as ibuprofen, are used to reduce inflammation, and your doctor may recommend them for several months. As your child progresses through the disease stages, your doctor will adjust or discontinue dosages.
Limiting activity. Avoiding high impact activities, such as running and jumping, will help relieve pain and protect the femoral head. Your doctor may also recommend crutches or a walker to prevent your child from putting too much weight on the joint.
Physical therapy exercises. Hip stiffness is common in children with Perthes disease and physical therapy exercises are recommended to help restore hip joint range of motion. These exercises often focus on hip abduction and internal rotation. Parents or other caregivers are often needed to help the child complete the exercises.
- Hip abduction. The child lies on his or her back, keeping knees bent and feet flat. He or she will push the knees out and then squeeze the knees together. Parents should place their hands on the child’s knees to assist with reaching a greater range of motion.
- Hip rotation. With the child on his or her back and legs extended out straight, parents should roll the entire leg inward and outward.

Casting and bracing. If range of motion becomes limited or if x-rays or other image scans indicate that a deformity is developing, a cast or brace may be used to keep the head of the femur in its normal position within the acetabulum.
Petrie casts are two long-leg casts with a bar that hold the legs spread apart in a position similar to the letter “A.” Your doctor will most likely apply the initial Petrie cast in an operating room in order to have access to specific equipment.
- Arthrogram. During the procedure, your doctor will take a series of special x-ray images called arthrograms to see the degree of deformity of the femoral head and to make sure he or she positions the head accurately. In an arthrogram, a small amount of dye is injected into the hip joint to make the anatomy even easier to see.
- Tenotomy. In some cases, the adductor longus muscle in the groin is very tight and prevents the hip from rotating into the proper position. Your doctor will perform a minor procedure to release this tightness — called a tenotomy — before applying the Petrie casts. During this quick procedure, your doctor uses a thin instrument to make a small incision in the muscle.
After the cast is removed, usually after 4 to 6 weeks, physical therapy exercises are resumed. Your doctor may recommend continued intermittent casting until the hip enters the final stage of the healing process.
Surgical Treatment
Your doctor may recommend surgery to re-establish the proper alignment of the bones of the hip and to keep the head of the femur deep within the acetabulum until healing is complete. Surgery is most often recommended when:
- Your child is older than age 8 at the time of diagnosis. Because the potential for deformity during the reossification stage is greater in older children, preventing damage to femoral head is even more critical.
- More than 50% of the femoral head is damaged. Keeping the femoral head within the rounded acetabulum may help the bone grow into a functional shape.
- Nonsurgical treatment has not kept the hip in correct position for healing.
The most common surgical procedure for treating Perthes disease is an osteotomy. In this type of procedure, the bone is cut and repositioned to keep the femoral head snug within the acetabulum. This alignment is kept in place with screws and plates, which will be removed after the healed stage of the disease.

In many cases, the femur bone is cut to realign the joint. Sometimes, the socket must also be made deeper because the head of the femur has actually enlarged during the healing process and no longer fits snugly within it. After either procedure, the child is usually placed in a cast for 6 to 8 weeks to protect the alignment.
After the cast is removed, physical therapy will be needed to restore muscle strength and range of motion. Crutches or a walker will be necessary to reduce weightbearing on the affected hip. Your doctor will continue to monitor the hip with x-rays through the final stages of healing.
Outcomes
In most cases, the long-term prognosis for children with Perthes is good and they grow into adulthood without further hip problems.
If there is deformity in the shape of the femoral head, there is more potential for future problems; however, if the deformed head still fits into the acetabulum, problems may be avoided. In cases where the deformed head does not fit well into the acetabulum, hip pain or early onset of arthritis is likely in adulthood.

Reviewed by members of the Pediatric Orthopaedic Society of North America
