Hip Fractures
A hip fracture is a break in the upper quarter of the femur (thigh) bone. The extent of the break depends on the forces that are involved. The type of surgery used to treat a hip fracture is primarily based on the bones and soft tissues affected or on the level of the fracture.
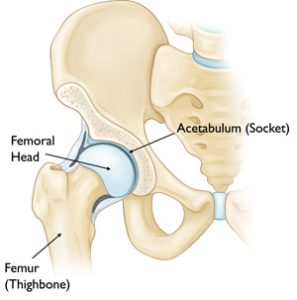
Anatomy
The “hip” is a ball-and-socket joint. It allows the upper leg to bend and rotate at the pelvis. An injury to the socket, or acetabulum, itself is not considered a “hip fracture.” Management of fractures to the socket is a completely different consideration.
Causes
Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting.
Symptoms
The patient with a hip fracture will have pain over the outer upper thigh or in the groin. There will be significant discomfort with any attempt to flex or rotate the hip.
If the bone has been weakened by disease (such as a stress injury or cancer), the patient may notice aching in the groin or thigh area for a period of time before the break. If the bone is completely broken, the leg may appear to be shorter than the noninjured leg. The patient will often hold the injured leg in a still position with the foot and knee turned outward (external rotation).
Doctor Examination
Imaging
The diagnosis of a hip fracture is generally made by an X-ray of the hip and femur.

In some cases, if the patient falls and complains of hip pain, an incomplete fracture may not be seen on a regular X-ray. In that case, magnetic resonance imaging (MRI) may be recommended. The MRI scan will usually show a hidden fracture.
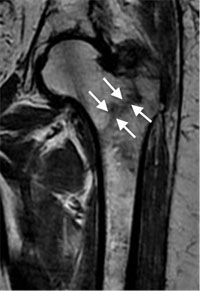
If the patient is unable to have an MRI scan because of an associated medical condition, computed tomography (CT) may be obtained instead. Computed tomography, however, is not as sensitive as MRI for seeing hidden hip fractures.
Types of Fractures
In general, there are three different types of hip fractures. The type of fracture depends on what area of the upper femur is involved.
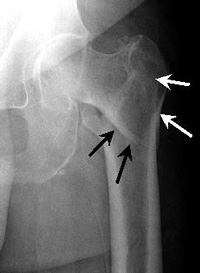
Intracapsular Fracture
These fractures occur at the level of the neck and the head of the femur, and are generally within the capsule. The capsule is the soft-tissue envelope that contains the lubricating and nourishing fluid of the hip joint itself.

Intertrochanteric Fracture
This fracture occurs between the neck of the femur and a lower bony prominence called the lesser trochanter. The lesser trochanter is an attachment point for one of the major muscles of the hip. Intertrochanteric fractures generally cross in the area between the lesser trochanter and the greater trochanter. The greater trochanter is the bump you can feel under the skin on the outside of the hip. It acts as another muscle attachment point.
Subtrochanteric Fracture
This fracture occurs below the lesser trochanter, in a region that is between the lesser trochanter and an area approximately 2 1/2 inches below .
In more complicated cases, the amount of breakage of the bone can involve more than one of these zones. This is taken into consideration when surgical repair is considered.
Treatment
Considerations
Once the diagnosis of the hip fracture has been made, the patient’s overall health and medical condition will be evaluated. In very rare cases, the patient may be so ill that surgery would not be recommended. In these cases, the patient’s overall comfort and level of pain must be weighed against the risks of anesthesia and surgery.
Most surgeons agree that patients do better if they are operated on fairly quickly. It is, however, important to insure patients’ safety and maximize their overall medical health before surgery. This may mean taking time to do cardiac and other diagnostic studies.
Nonsurgical Treatment
Patients who might be considered for nonsurgical treatment include those who are too ill to undergo any form of anesthesia and people who were unable to walk before their injury and may have been confined to a bed or a wheelchair.
Certain types of fractures may be considered stable enough to be managed with nonsurgical treatment. Because there is some risk that these “stable” fractures may instead prove unstable and displace (change position), the doctor will need to follow with periodic X-rays of the area. If patients are confined to bed rest as part of the management for these fractures, they will need to be closely monitored for complications that can occur from prolonged immobilization. These include infections, bed sores, pneumonia, the formation of blood clots, and nutritional wasting.

Surgical Treatment
Before Surgery
Anesthesia for surgery could be either general anesthesia with a breathing tube or spinal anesthesia. In very rare circumstances, where only a few screws are planned for fixation, local anesthesia with heavy sedation can be considered. All patients will receive antibiotics during surgery and for the 24-hours afterward.
Appropriate blood tests, chest X-rays, electrocardiograms, and urine samples will be obtained before surgery. Many elderly patients may have undiagnosed urinary tract infections that could lead to an infection of the hip after surgery.
The surgeon’s decision as to how to best fix a fracture will be based on the area of the hip that is broken and the surgeon’s familiarity with the different systems that are available to manage these injuries.
Intracapsular Fracture
If the head of the femur (“ball”) alone is broken, management will be aimed at fixing the cartilage on the ball that has been injured or displaced. Frequently with these injuries, the socket, or acetabulum, may also be broken. The surgeon will need to take this into consideration as well.
These injuries may be approached either from either the front or back of the hip. In some cases, both approaches are required in order to clearly see and fix the injured bone.
For true intracapsular hip fractures, the surgeon may decide either to fix the fracture with individual screws (percutaneous pinning) or a single larger screw that slides within the barrel of a plate. This compression hip screw will allow the fracture to become more stable by having the broken area impact on itself. Occasionally, a secondary screw may be added for stability.


If the intracapsular hip fracture is displaced in a younger patient, a surgical attempt will be made to reduce, or realign, the fracture through a larger incision. The fracture will be held together with either individual screws or with the larger compression hip screw.
In these cases, the blood supply to the ball, or head of the femur, may have been damaged at the time of injury (avascular necrosis). Even though the fracture is realigned and fixed into place, the cartilage and underlying supporting bone may not receive adequate blood. Over a period of time, this may cause the femoral head to flatten out. When this occurs, the joint surface becomes irregular. Ultimately, the hip joint may develop a painful arthritis, despite the surgical repair.

In the older patient, the chance that the head of the femur is damaged in this way is higher. It is generally felt that for these displaced fractures, patients will do better if some of the components of the hip are replaced. In some cases, this can mean a replacement of the ball, or head of the femur (hemiarthroplasty). In other cases, this can mean the replacement of both the ball and socket, or head of the femur and acetabulum (total hip replacement).


Intertrochanteric Fracture
Most intertrochanteric fractures are managed with either a compression hip screw or an intramedullary nail, which also allows for impaction at the fracture site.
The compression hip screw is fixed to the outer side of the bone with bone screws and has a large secondary screw (lag screw) that is placed through the plate into the neck and head of the hip (see compression hip screw figure above). The design of the device allows for impaction and compression at the fracture site. This may increase the stability of the area and promote healing.
The intramedullary nail is placed directly into the marrow canal of the bone through an opening made at the top of the greater trochanter. A lag screw is then placed through the nail and up into the neck and head of the hip. As with the compression hip screw, sliding of the lag screw and impaction of the fracture take place.

There are no definitive studies to show that one device is superior to another. The decision as to which to use is based on the surgeon’s preference and experience.
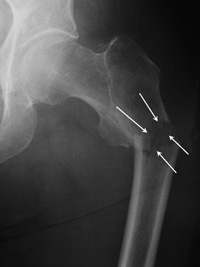
Subtrochanteric Fracture
At the subtrochanteric level, most fractures are managed with a long intramedullary nail together with a large lag screw or they are managed with screws that capture the neck and head of the femur or the area immediately underneath it, if it has remained intact.


In order to keep the bones from rotating around the nail or from shortening (“telescoping”) on the nail, additional screws may be placed at the lower end of the nail in the area of the knee. These are called interlocking screws.
In certain cases, the surgeon may choose to use a plate rather than a nail. The plate will have screws that go into the bone from the lateral, or outer, side of the femur. A single large screw goes into the neck and the head of the femur and appears similar to the compression hip screw, but at a different angle. Secondary screws are then placed through the plate into the bone to hold the fracture in place.

Recovery
Patients may be discharged from the hospital to their home or find that a stay in a rehabilitation facility is necessary to assist them in regaining their ability to walk.
Pain Management
Pain after an injury or surgery is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover faster.
Medications are often prescribed for short-term pain relief after surgery or an injury. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your treatment.
Rehabilitation
Patients may be encouraged to get out of bed on the day following surgery with the assistance of a physical therapist. The amount of weight that is allowed to be placed on the injured leg will be determined by the surgeon and is generally a function of the type of fracture and repair (fixation).
The physical therapist will work with the patient to help regain strength and the ability to walk. This process may take up to three months.
Medical Care
Occasionally, a blood transfusion may be required after surgery, but longer term antibiotics are generally not necessary.
Most patients will be placed on medicine to thin their blood to reduce the chances of developing blood clots for up to 6 weeks. These medicines may be in the form of pills or injections. Elastic compression stockings or inflatable compression boots may also be used.
Follow-Up Care
During the appointments that take place after surgery, the surgeon will want to check the wound, remove sutures, follow the healing process using X-rays, and prescribe additional physical therapy, if necessary.
Following hip fracture surgery, most patients will regain much, if not all, of the mobility and independence they had before the injury.
For More Information
If you found this article helpful, you may also be interested in Fractures (Broken Bones).
In order to assist doctors in the management of hip fractures in the elderly, the American Academy of Orthopaedic Surgeons has done research to provide some useful guidelines. These are recommendations only and may not apply to each and every individual case. For more information: AAOS Clinical Practice Guideline: Management of Hip Fractures in the Elderly.
![]()
Co-developed by the Orthopaedic Trauma Association
