Pelvic Fractures
The pelvis is the sturdy ring of bones located at the base of the spine. Fractures of the pelvis are uncommon—accounting for only about 3% of all adult fractures.
Most pelvic fractures are caused by some type of traumatic, high-energy event, such as a car collision. Because the pelvis is in proximity to major blood vessels and organs, pelvic fractures may cause extensive bleeding and other injuries that require
urgent treatment.
In some cases, a lower-impact event—such as a minor fall—may be enough to cause a pelvic fracture in an older person who has weaker bones.
Treatment for a pelvic fracture varies depending on the severity of the injury. While lower-energy fractures can often be managed with conservative care, treatment for high-energy pelvic fractures usually involves surgery to reconstruct the pelvis and restore stability so that patients can resume their daily activities.
Anatomy
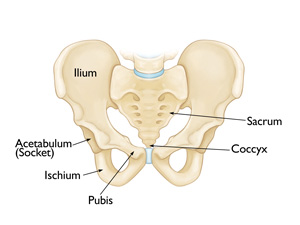
The pelvis is a ring of bones located at the lower end of the trunk—between the spine and the legs. The pelvic bones include the:
- Sacrum (the large triangular bone at the base of the spine)
- Coccyx (tailbone)
- Hip bones
Each hip bone contains three bones—the ilium, ischium, and pubis—that are separate during childhood but fuse together as we grow older. These three bones meet to form the acetabulum—the hollow cup that serves as the socket for the ball-and-socket hip joint.
Bands of strong connective tissues called ligaments join the pelvis to the sacrum, creating a bowl-like cavity below the rib cage.
Major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs all pass through the pelvic ring. The pelvis protects these important structures from injury. It also serves as an anchor for the muscles of the hip, thigh, and abdomen.
Description
Because the pelvis is a ring-like structure, a fracture in one part of the structure is often accompanied by a fracture or damage to ligaments at another point in the structure. Doctors have identified several common pelvic fracture patterns. The specific pattern of the fracture depends upon the direction in which it was broken and the amount of force that caused the injury.
In addition to being described by the specific fracture pattern, pelvic fractures are often described as “stable” or “unstable,” based on how much damage has occurred to the structural integrity of the pelvic ring.
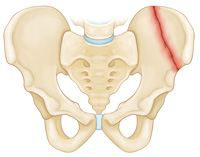
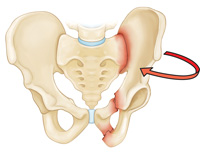
Stable fracture. In this type of fracture, there is often only one break in the pelvic ring and the broken ends of the bones line up adequately. Low-energy fractures are often stable fractures. Stable pelvic fracture patterns include:
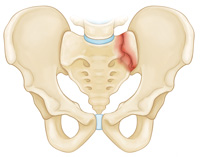
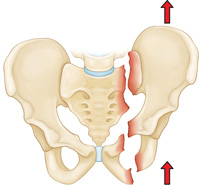
Unstable fracture. In this type of fracture, there are usually two or more breaks in the pelvic ring and the ends of the broken bones do not line up correctly (displacement). This type of fracture is more likely to occur due to a high-energy event. Unstable pelvic fracture patterns include:
Both stable and unstable pelvic fractures can also be divided into “open” fractures, in which the bone fragments stick out through the skin, or “closed” fractures, in which the skin is not broken. Open fractures are particularly serious because, once the skin is broken, infection in both the wound and the bone can occur. Immediate treatment is required to prevent infection.
Cause
High-Energy Trauma
A pelvic fracture may result from a high-energy force, such as that generated during a:
- Car or motorcycle collision
- Crush accident
- Fall from a significant height (such as a ladder)
Depending on the direction and magnitude of the force, these injuries can be life-threatening and require surgical treatment.
Bone Insufficiency
A pelvic fracture may also occur due to weak or insufficient bone. This is most common in older people whose bones have become weakened by osteoporosis. In these patients, a fracture may occur even during a fall from standing or a routine activity such as getting out of the bathtub or descending stairs. These injuries are typically stable fractures that do not damage the structural integrity of the pelvic ring, but may fracture an individual bone.
Other Causes
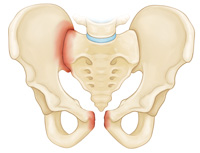
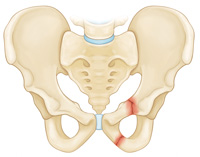
Less commonly, a fracture may occur when a piece of the ischium bone tears away from the site where the hamstring muscles attach to the bone. This type of fracture is called an avulsion fracture and it is most common in young athletes who are still growing. An avulsion fracture does not usually make the pelvis unstable or injure internal organs.
Symptoms
A fractured pelvis is almost always painful. This pain is aggravated by moving the hip or attempting to walk. Often, the patient will try to keep his or her hip or knee bent in a specific position to avoid aggravating the pain. Some patients may experience swelling or bruising in the hip area.
Doctor Examination
Emergency Stabilization
Patients with high-energy fractures will almost always go or be brought to an urgent care center or emergency room for initial treatment due to the severity of their symptoms.
These patients may also have additional injuries to the head, chest, abdomen, or legs. If their injuries cause significant blood loss, it could lead to shock—a life-threatening condition that can result in organ failure.
The care of patients with high-energy pelvic fractures requires a multidisciplinary approach with input from a number of medical specialists. In some cases, doctors must address airway, breathing, and circulatory problems before treating the fracture and other injuries.
Physical Examination
Your doctor will carefully examine your pelvis, hips, and legs. He or she will also check for nerve injury by assessing whether you can move your ankles and toes and feel sensation on the bottom of your feet.
Your doctor will also carefully examine the rest of your body to determine if you have sustained any other injuries.
Imaging Studies
X-rays. These studies provide images of dense structures, such as bones. All pelvic fractures require x-rays—usually from a number of different angles—to help the doctor determine how displaced place the bones are.

Computed tomography (CT) scans. Because of the complexity of this type of injury, a CT scan is commonly ordered for pelvic fractures. A CT scan will provide a more detailed, cross-sectional image of the pelvis. Your doctor will use this information to better determine the specific pattern and extent of your injury, look for associated injuries, and aid in preoperative planning.
Magnetic resonance imaging (MRI) scans: In rare cases, your doctor may order an MRI scan to discover a fracture that cannot be seen on x-ray or CT scan.
Treatment
Treatment is based on a number of factors, including:
- The specific pattern of the fracture
- How much the bones are displaced
- Your overall condition and associated injuries
Nonsurgical Treatment
Your doctor may recommend nonsurgical treatment for stable fractures in which the bones are nondisplaced or minimally displaced.
Nonsurgical treatments may include:
Walking aids. To avoid bearing weight on your leg, your doctor may recommend that you use crutches or a walker for up to three months—or until your bones are fully healed. If you have injuries above both legs, you may need to use a wheelchair for a period of time so that you can avoid bearing weight on either leg.
Medications. Your doctor may prescribe medication to relieve pain, as well as an anti-coagulant, or blood thinner, to reduce the risk of blood clots forming in the veins of your legs and pelvis.
Surgical Treatment
Patients with unstable pelvic fractures may require one or more surgical procedures.
External fixation. Your doctor may use external fixation to stabilize your pelvic area. In this operation, metal pins or screws are inserted into the bones through small incisions into the skin and muscle. The pins and screws project out of the skin on both sides of the pelvis where they are attached to carbon fiber bars outside the skin. The external fixator acts as a stabilizing frame to hold the broken bones in proper position.
In some cases, an external fixator is used to stabilize the bones until healing is complete. In patients who are unable to tolerate a lengthy, more complicated procedure, an external fixator may be used as a temporary treatment until another procedure can be performed.

Skeletal traction. Skeletal traction is a pulley system of weights and counterweights that helps realign the pieces of bone. Skeletal traction is often used immediately after an injury and removed after surgery. Occasionally, acetabular fractures can be treated with skeletal traction alone. This is rare, however, and will be a decision made jointly with input from your doctor.
During skeletal traction, metal pins are implanted in the thighbone or shinbone to help position the leg. Weights attached to the pins gently pull on the leg, keeping the broken bone fragments in as normal a position as possible. For many patients, skeletal traction also provides some pain relief.
Open reduction and internal fixation. During this operation, the displaced bone fragments are first repositioned (reduced) into their normal alignment. They are then held together with screws or metal plates attached to the outer surface of the bone.

Complications
There are risks associated with any surgical procedure. Before your surgery, your doctor will discuss each of these risks with you and will take specific measures to help avoid potential complications.
Possible complications include:
- Wound healing problems, including infection
- Damage to nerves or blood vessels
- Blood clots
- Pulmonary embolism—a blood clot in the lungs
Recovery
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Early Movement
In most cases, your doctor will encourage early movement. Most patients begin walking—with weight-bearing restrictions—and performing foot and leg exercises as soon as possible after surgery.
Physical Therapy
Specific exercises will help you regain flexibility and restore range of motion in your hip. Other exercises will help you build strength and endurance so that you are better able to perform your daily activities.
Blood Clot Prevention
Although early movement is encouraged, your mobility after surgery will still be somewhat limited. For this reason, your doctor may prescribe an anticoagulant, or blood thinner, to help prevent blood clots from forming in the deep veins of your pelvis and legs.
Weight Bearing
Your doctor may recommend that you use crutches or a walker for a period of time. Full weight bearing is usually allowed by 3 months—or when your bones are fully healed. You may require the use of a cane or walking aid for a longer period of time.
Outcomes
Stable pelvic fractures tend to heal well. Unstable pelvic fractures sustained during high-energy incidents, such as car accidents, may result in significant complications, including severe bleeding, internal organ damage, and infection. If these injuries are addressed successfully, the fracture usually heals well.
You may walk with a limp for several months if damage has occurred to the muscles around your pelvis. These muscles may take up to one year to become strong again.
Subsequent problems, such as pain, impaired mobility, and sexual dysfunction, may result from damage to nerves and organs that is associated with the pelvic fracture.
If you found this article helpful, you may also be interested in Deep Vein Thrombosis.